Researchers report identifying the “fingerprint” of the immune cells that characterize multiple sclerosis.
They say the discovery could lead to new ways to monitor and treat the disease.
In patients with multiple sclerosis (MS), dysregulated immune cells periodically infiltrate the brain, causing damage to neural transmission and neuronal loss. Without proper monitoring and treatment, the disease leads to accumulating disabilities that ultimately greatly restrict the daily life of patients.
Around 2.5 million people, many young adults, suffer from the chronic autoimmune disease.
“We identified a specific population of white blood cells augmented in the peripheral blood of MS patients that have two properties characteristic of MS: They can move from the blood to the central nervous system and there they can cause inflammation of the nerve cells,” says Burkhard Becher at the Institute of Experimental Immunology of the University of Zurich.
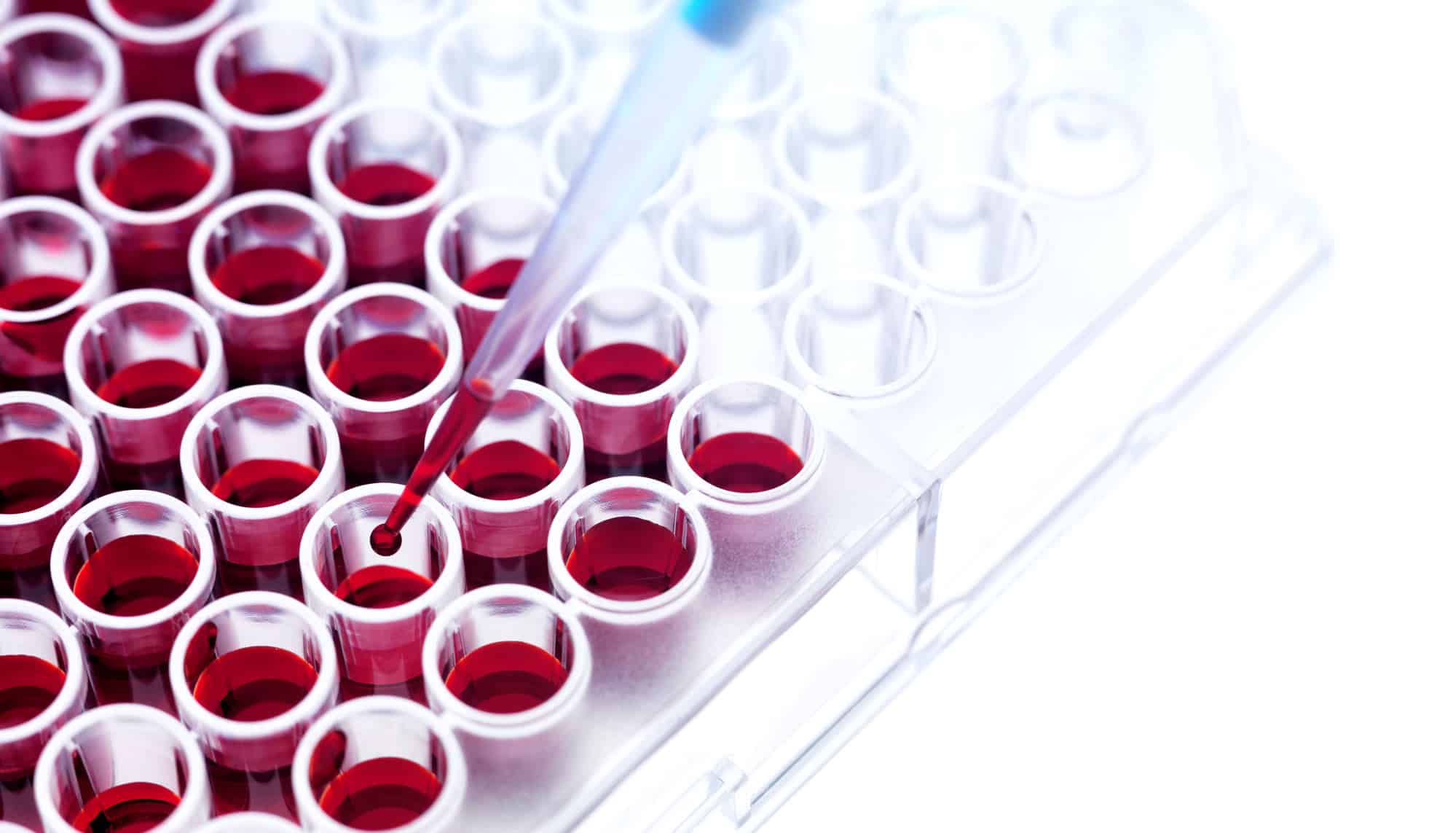
For the study in Nature Medicine, researchers used high-dimensional cytometry to characterize the immune cells. The technology makes it possible to analyze millions of cells in hundreds of patients and determine their immune properties—in other words, their “fingerprints.”
To analyze the enormous amount of data, the scientists developed an innovative machine-learning algorithm.
“Artificial intelligence and machine learning helps us to greatly reduce the data’s complexity, while the interpretation of results is left to the investigators,” Becher says.
The team identified a population of immune cells in the peripheral blood of MS patients that differ from those in other inflammatory and non-inflammatory diseases. These dysregulated T helper cells produce a neuroinflammatory cytokine called GM-CSF and high levels of the chemokine receptor CXCR4 and the membrane protein VLA4.
“The cell population we identified therefore has two key properties that are characteristic of MS: The cytokine causes neuroinflammation, and thanks to the receptors the immune cells can get into the central nervous system,” says first author Edoardo Galli.
In addition, the researchers found this characteristic signature to be highly represented in the cerebrospinal fluid and in the brain lesions of MS patients, suggesting a direct contribution to the disease. Effective immunomodulatory therapy strongly reduces this cell population.
“Our data clearly indicate a stringent association of this signature to MS, and we believe that the identification of such an easily accessible biomarker brings important value for MS monitoring,” Becher says.
While it’s still premature to claim a disease-causing role for this population—and further studies are needed to confirm the hypothesis—the findings could provide important hints for new MS-specific treatments to improve the patients’ care, the researchers say.
Source: University of Zurich