The deadly new coronavirus is spreading faster in America’s jails and prisons than it did on the Princess Diamond cruise ship or at the pandemic’s outbreak in Wuhan, China, research finds.
Why? Few opportunities for social distancing and relatively low sanitary conditions.
“These interventions include depopulation, increased single celling, and widespread testing of asymptomatic people who are incarcerated.”
The research, which appears in the journal Annals of Epidemiology, is based on day-by-day data from a large urban jail and highlights the health risk that correctional institutions pose during the current crisis—not just to inmates and staff but also to surrounding communities.
Here, two Stanford University coauthors of the study speak about the broader implications. Margaret L. Brandeau, a professor of management sciences and engineering, has spent much of her career analyzing strategies to slow the spread of diseases such as HIV and hepatitis C. Giovanni Malloy is a PhD candidate who works on infectious disease models.
How was this study conducted?
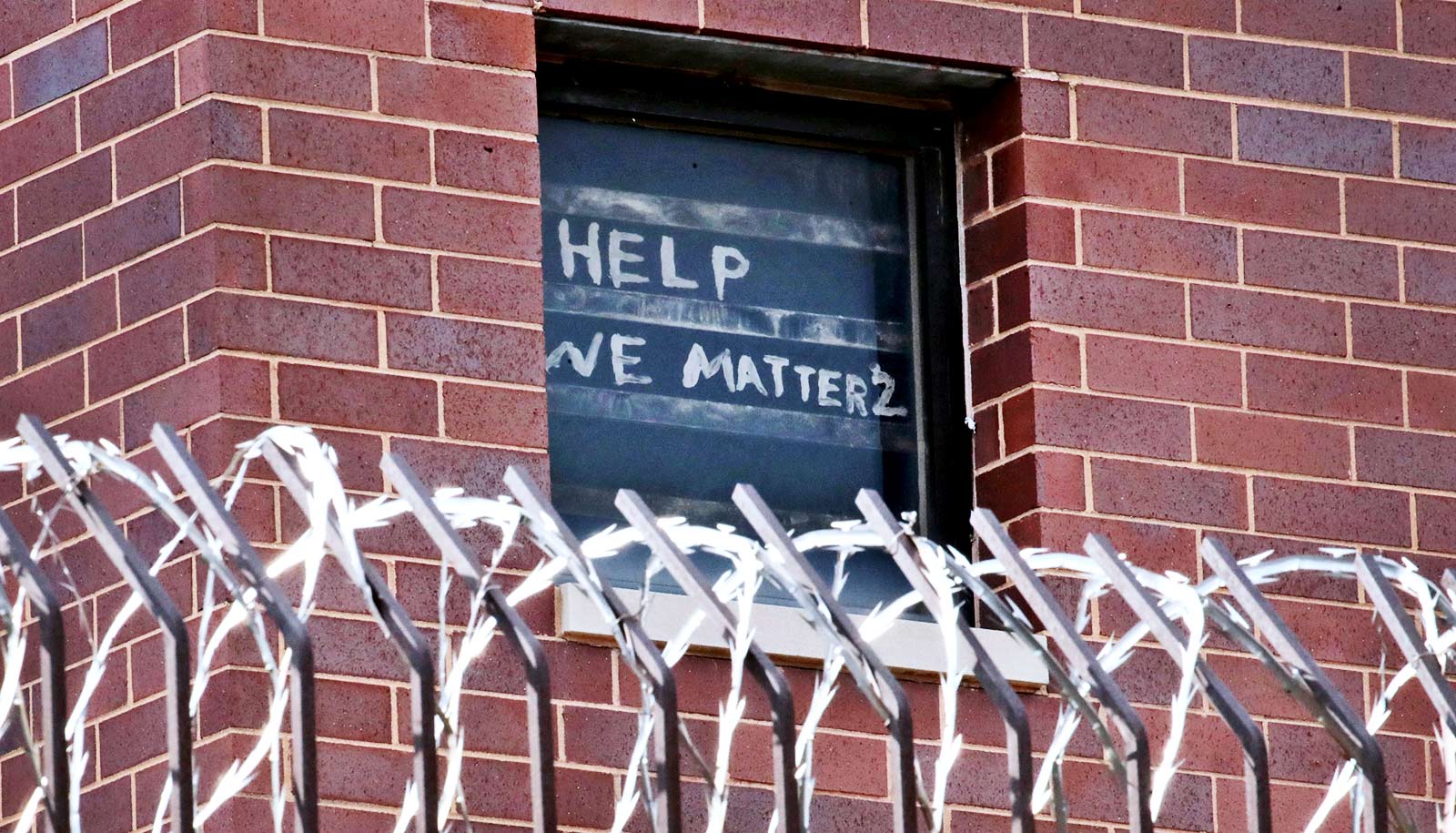
We knew that prisons and jails had become hot spots for the novel coronavirus because there’s very little opportunity for social distancing—it’s common to have two or more people per cell—and sanitary conditions are comparatively low. But we wanted to know precisely how fast it was spreading.
We teamed up with Lisa Puglisi at the Yale School of Medicine, who has long specialized in the health issues of people who are incarcerated. We worked with a large urban jail, which is remaining anonymous, to analyze the daily tallies of people who were testing positive, as well as of people who did and did not become sick, and of people who recovered or died.
After running roughly 1,000 computer simulations based on those numbers, we concluded that each infected person was spreading the virus to 8.44 other people at the very beginning of the outbreak. To put that in perspective, the virus spread 3.6 times faster in this jail than it did aboard the Princess Diamond in February and over 4 times faster than in Wuhan.
Do you think this is typical for other jails and prisons?
This study may actually understate the speed of infection at these institutions. That’s because this jail was unusually quick in taking steps to slow the virus’s spread. Very soon after the first person became sick, for example, the jail began releasing about 1% of inmates per day in order to have more room to separate those who had become infected, which we estimate reduced transmission by 56% as compared to the initial outbreak. At the many correctional facilities that haven’t moved as quickly, the virus is very likely spreading faster.
There is no question that jails are an epicenter of COVID-19 transmission in the United States, and it’s essential that we take measures to control its spread in these settings. Cook County Jail in Illinois had one of the largest known outbreaks in the country, and the infection rate at Rikers Island is nearly five times that of New York City. Across Texas, 70% of inmates and staff who were tested in April turned out to be positive. At the state prison in Marion, Ohio, 73% of those tested were positive.
Do jails and prisons pose a risk outside their own walls?
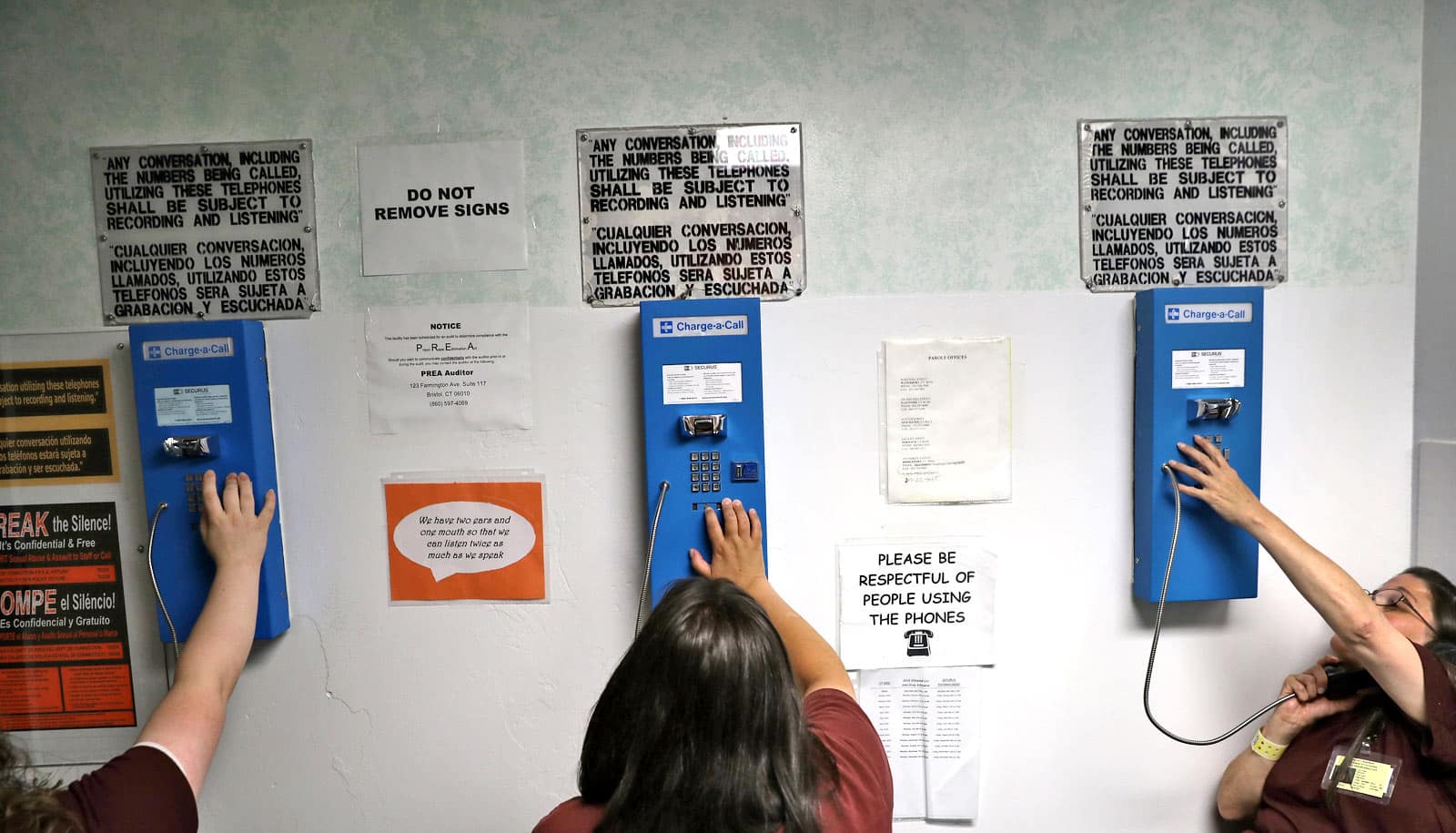
Most certainly. The people who work there enter and leave every day. They can take the virus out into the community when they go home at night. It’s also important to remember that correctional institutions have been exempted from current federal guidelines aimed at protecting people in workplaces and in large housing complexes. There are many reasons to be concerned about this, beyond the dangers to the people inside.
What measures can correctional facilities take to limit the danger?
After our initial report on calculating the basic reproduction number of the initial outbreak, we continued to work with the jail to identify the effectiveness of three different interventions they implemented on top of CDC interim guidelines. These interventions include depopulation, increased single celling, and widespread testing of asymptomatic people who are incarcerated. Using data from our jail partner, we estimated that each of these interventions can individually reduce transmission by over 50%. In combination, they will effectively lead to the end of an outbreak.
Depopulation is an important measure to attempt to achieve a higher degree of socially distancing in jails and prisons. Jails, which generally hold people while they await trial, have more flexibility in releasing people than prisons. But even for jails, these are difficult decisions. Depopulation requires a coordinated effort on the part of police departments, judges, correctional departments, lawyers, and community bail funds to reduce jail intakes and/or increase releases. Depopulation efforts pave the way to make single celling more feasible such that a greater portion of people who are incarcerated will be assigned to their own cell.
Finally, asymptomatic testing is critical to COVID-19 mitigation. A very high percentage of those who are infected—perhaps 40%—don’t show any symptoms at all. Without sufficient testing, a jail won’t know how serious its problems are and it won’t know which people to prioritize for single-person cells and isolate from the rest of the population.
Source: Stanford University