People with asthma seem to be less likely to develop brain tumors than others and now researchers believe they’ve discovered why via a study of mice.
It comes down to the behavior of T cells, a type of immune cell. When a person—or a mouse—develops asthma, a breathing disease in which the airways become narrowed and inflamed, their T cells become activated.
“These findings open the door to new kinds of therapies targeting T cells and their interactions with cells in the brain.”
In a new mouse study, researchers discovered that asthma causes the T cells to behave in a way that induces lung inflammation but prevents the growth of brain tumors. What’s bad news for the airways may be good news for the brain.
The findings suggest that reprogramming T cells in brain tumor patients to act more like T cells in asthma patients could be a new approach to treating brain tumors.
“Of course, we’re not going to start inducing asthma in anyone; asthma can be a lethal disease,” says senior author David H. Gutmann, professor of neurology at Washington University in St. Louis. “But what if we could trick the T cells into thinking they’re asthma T cells when they enter the brain, so they no longer support brain tumor formation and growth? These findings open the door to new kinds of therapies targeting T cells and their interactions with cells in the brain.”
The idea that people with inflammatory diseases, such as asthma or eczema, are less prone to developing brain tumors was first proposed more than 15 years ago, based on epidemiologic observations. But there was no obvious reason why the two very different kinds of diseases would be linked, and some scientists questioned whether the association was real.
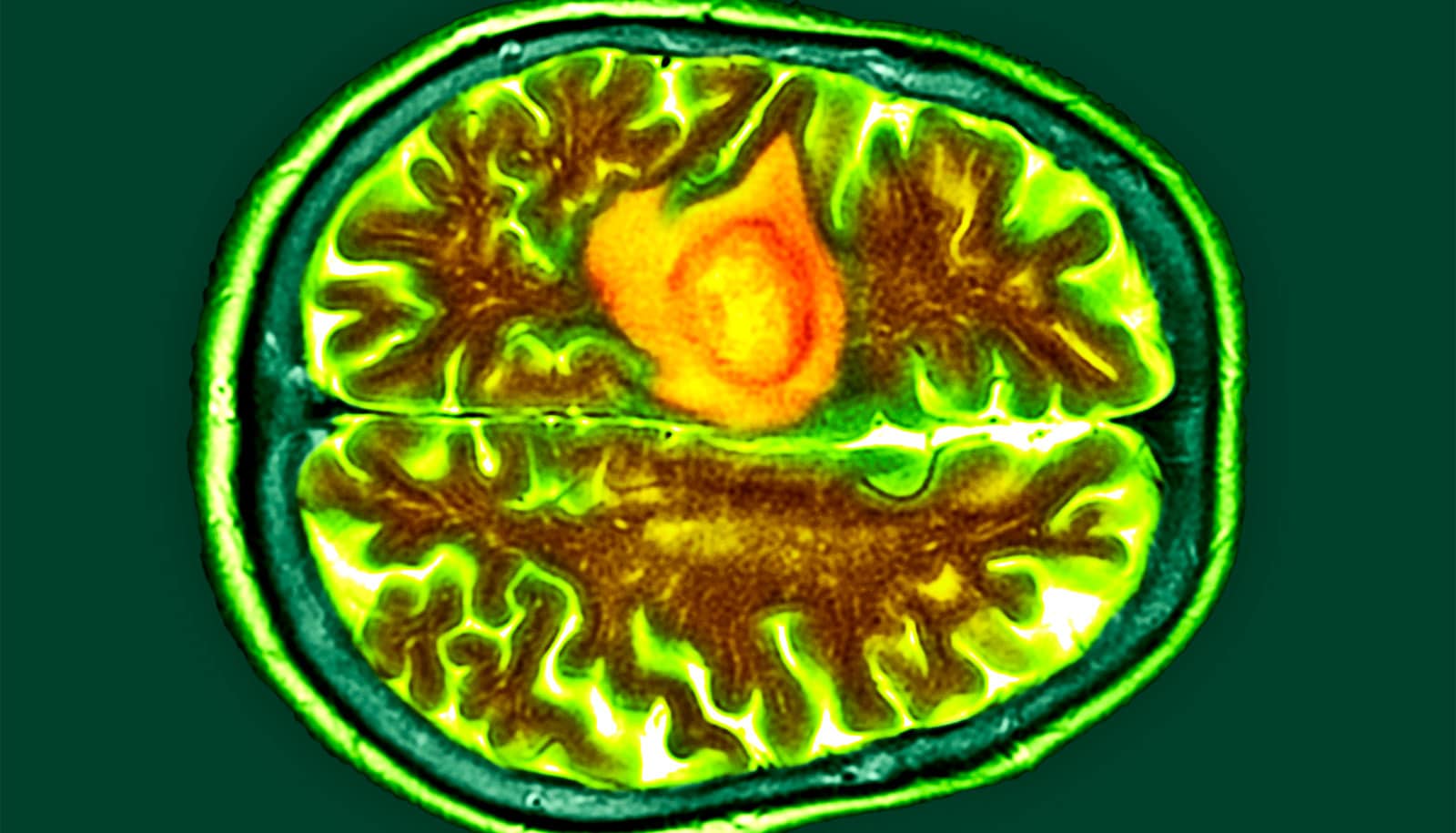
Gutmann is an expert on neurofibromatosis (NF), a set of complex genetic disorders that cause tumors to grow on nerves in the brain and throughout the body. Children with NF type 1 (NF1) can develop a kind of brain tumor known as an optic pathway glioma. These tumors grow within the optic nerves, which carries messages between the eyes and the brain.
Gutmann noted an inverse association between asthma and brain tumors among his patients more than five years ago but didn’t know what to make of it. It wasn’t until more recent studies from his lab began to reveal the crucial role that immune cells play in the development of optic pathway gliomas that he began to wonder whether immune cells could account for the association between asthma and brain tumors.
Jit Chatterjee, a postdoctoral researcher and the paper’s first author, took on the challenge of investigating the association. Working with coauthor Michael J. Holtzman, professor of medicine and director of the Division of Pulmonary & Critical Care Medicine, Chatterjee studied mice genetically modified to carry a mutation in their NF1 genes and form optic pathway gliomas by 3 months of age.
Chatterjee exposed groups of mice to irritants that induce asthma at age 4 weeks to 6 weeks, and treated a control group with saltwater for comparison. Then, he checked for optic pathway gliomas at 3 months and 6 months of age. The mice with asthma did not form these brain tumors.
Further experiments revealed that inducing asthma in tumor-prone mice changes the behavior of their T cells. After the mice developed asthma, their T cells began secreting a protein called decorin that is well-known to asthma researchers.
In the airways, decorin is a problem. It acts on the tissues that line the airways and exacerbates asthma symptoms. But in the brain, Chatterjee and Gutmann discovered, decorin is beneficial. There, the protein acts on immune cells known as microglia and blocks their activation by interfering with the NFkappaB activation pathway. Activated microglia promote the growth and development of brain tumors.
Treatment with either decorin or caffeic acid phenethyl ester (CAPE), a compound that inhibits the NFkappaB activation pathway, protected mice with NF1 mutations from developing optic pathway gliomas. The findings suggest that blocking microglial activation may be a potentially useful therapeutic approach for brain tumors.
“The most exciting part of this is that it shows that there is a normal communication between T cells in the body and the cells in the brain that support optic pathway glioma formation and growth,” says Gutmann, who is also a professor of genetics, of neurosurgery, and of pediatrics.
“The next step for us is to see whether this is also true for other kinds of brain tumors. We’re also investigating the role of eczema and early-childhood infections, because they both involve T cells. As we understand this communication between T cells and the cells that promote brain tumors better, we’ll start finding more opportunities to develop clever therapeutics to intervene in the process.”
The research appears in Nature Communications.
Funding for the work came from the National Institute of Neurological Disorders and Stroke of the National Institutes of Health (NIH); the National Heart, Lung, and Blood Institute of the NIH; and a POST grant from Alex’s Lemonade Stand Foundation.