A simple blood test to diagnose Alzheimer’s disease may soon replace more invasive and expensive screening methods such as spinal taps and brain scans, a new study shows.
The findings show that a blood test can be as good at detecting molecular signs of Alzheimer’s disease in the brain as cerebrospinal fluid tests approved by the Food and Drug Administration (FDA) for Alzheimer’s diagnosis. The blood test uses a highly sensitive technique to measure levels of Alzheimer’s proteins in the blood.
The research is published in Nature Medicine.
The findings demonstrate that a blood test can diagnose Alzheimer’s disease pathology as accurately as cerebrospinal fluid tests and brain scans, even in patients with mild symptoms, and can be used to detect molecular signs of Alzheimer’s disease in the brain when symptoms haven’t yet emerged.
Identifying people with the disease has become vitally important, as the first Alzheimer’s treatments capable of slowing the disease’s progression recently became available to patients, and other promising drugs are in the pipeline. Such drugs might be more effective when started sooner rather than later, making it critically important to identify people with the disease early.
“The accuracy of this blood test now enables us to diagnose the presence of Alzheimer’s disease pathology with a single blood sample,” says co-senior author Randall J. Bateman, professor of neurology at Washington University in St. Louis. “This advance will increase accurate diagnoses for many patients.”
For many years, Alzheimer’s was diagnosed symptomatically, after people began showing signs of memory and thinking problems. But studies have shown that up to a third of people diagnosed with Alzheimer’s based on cognitive symptoms alone are misdiagnosed and that their symptoms are due to other causes.
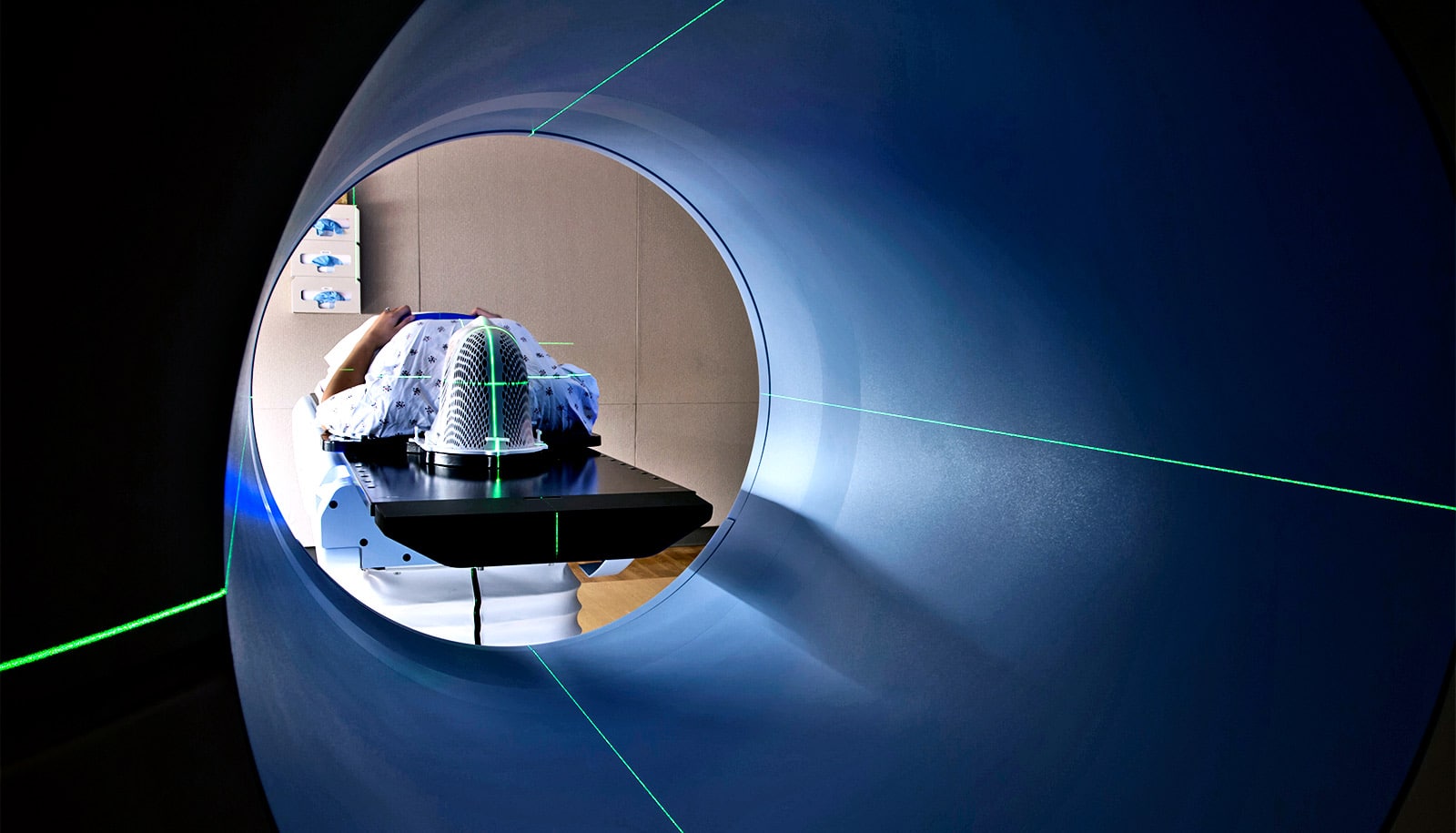
Consequently, before a patient is eligible to receive Alzheimer’s therapies, a diagnosis of cognitive impairment must be coupled with a positive test for amyloid plaques, which are unique to Alzheimer’s disease. Amyloid positron emission tomography (PET) brain scans, cerebrospinal fluid analyses, and blood tests can all be used to confirm the presence of brain amyloid plaques, but only for people who already have cognitive symptoms. They are not used by doctors for people without symptoms.
“In the near future, this type of blood test will replace the need for costly and less accessible cerebrospinal fluid and PET imaging tests in specialist memory clinics,” says co-senior author Oskar Hansson, a professor of neurology at Lund University. “Next, we need to determine if the Alzheimer’s blood test also works in primary care. This is currently being investigated in Sweden.”
Bateman and colleagues previously created the first approved blood test for amyloid in the brain that uses mass spectrometry to measure the ratio of two forms of amyloid in the blood. It received a “Breakthrough Device” designation from the FDA in 2019.
Bateman, co-first author Nicolas Barthélemy, an assistant professor of neurology at Washington University, and colleagues have since created a second blood test based on the effects of amyloid accumulation on a second brain protein: tau.
The presence of amyloid in the brain changes the levels of various forms of tau protein in the brain and in the blood. Measuring the ratio of phosphorylated tau-217 (ptau-217) and unphosphorylated tau in the blood reliably reflects brain amyloid levels.
A test combining the amyloid and tau blood measures is marketed by the Washington University startup C2N Diagnostics, as PrecivityAD2.
In this study, a research team led by Bateman, Hansson, Barthélemy, co-first author Gemma Salvadó, a postdoctoral fellow at Lund University, and coauthor Suzanne Schindler, an associate professor of neurology at Washington University, compared the abilities of four tests to identify people with amyloid in their brains: the ptau-217 blood test and three FDA-approved cerebrospinal fluid tests.
They evaluated the tests using blood and cerebrospinal fluid samples from volunteers in the Swedish BioFINDER-2 (Biomarkers For Identifying Neurodegenerative Disorders Early and Reliably) cohort (1,422 people), and Washington University’s Charles F. and Joanne Knight Alzheimer Disease Research Center (Knight ADRC) cohort (337 people). Both groups included people with very mild and mild cognitive symptoms, as well as healthy people for comparison. The tests’ accuracy rates were calculated by comparing their results to the gold standard: PET brain scans for amyloid and tau tangles.
The ptau-217 blood test was just as good as the FDA-approved cerebrospinal fluid tests at identifying people with amyloid buildup, with accuracy scores for all tests at 95% to 97%. In a secondary analysis, the researchers measured how well the tests determined the levels of tau tangles in the brain. In this, the ptau-217 blood test was superior to cerebrospinal fluid tests, with accuracy scores in the range of 95% to 98%.
As of now, Alzheimer’s therapies and diagnostic tests are only used clinically for people who already show signs of memory and thinking problems. But Alzheimer’s disease has a long presymptomatic phase of two decades or more during which amyloid builds up in the brain before neurodegeneration sets in and symptoms arise.
“We now have therapies that have clinical benefits, which is great, but they don’t reverse the loss of neurons in the brain,” Barthélemy says. “What we really want is to treat the disease before people start losing brain cells and showing symptoms.”
A subgroup analysis of healthy participants showed that the ptau-217 blood test accurately identified those who harbored amyloid plaques in their brains. The test was just as accurate at detecting the presence of amyloid plaques in people without symptoms as those with symptoms. Studies have shown that people with no cognitive problems but who are positive for amyloid are at high risk of developing cognitive impairments in the next few years.
A major phase 3 clinical trial known as the AHEAD 3-45 Study was launched in 2020 to evaluate whether treating amyloid-positive people before symptoms arise can prevent cognitive decline. Washington University is a site for the trial. The blood test is being used in the AHEAD study to screen potential participants.
“Imagine a person who is 55 or 60 and has a family history of Alzheimer’s or some high-risk genetic variants,” Barthélemy says. “It would be really valuable to have an easy way to know whether they have amyloid pathology in their brains.
“If they do, they could come in, maybe once every two or three years, and get a therapy to clear the amyloid out and then never develop dementia at all. We’re still a few years away from such an approach, but I think that’s the future of Alzheimer’s care, and it depends on presymptomatic diagnosis and treatment.”