Brain imaging to detect Alzheimer’s-related plaques affects clinical diagnosis and management of patients with mild cognitive impairment and dementia, according to a new study.
The findings, which appear in in the Journal of the American Medical Association, are a step toward understanding how imaging results ultimately affect patient outcomes. The study included 11,409 Medicare beneficiaries, 595 different clinical sites, and 946 dementia specialists.
The team found that providing clinicians with the results of positron emission tomography (PET) scans that identify amyloid plaques in the brain changed medical management—including the use of medications and counseling about dementia risks—in more than 60 percent of patients. This information also altered the diagnosis as to the cause of cognitive impairment in more than one in three study participants.
Here, Constantine Gatsonis, a professor of biostatistics in Brown University’s School of Public Health, shares insights on the Imaging Dementia—Evidence for Amyloid Scanning (IDEAS) study and his role as lead statistician.
What is the overall goal of the IDEAS study?
Currently, the Centers for Medicare and Medicaid Services (CMS) does not provide financial coverage for amyloid PET scans—they need more clinical evidence. The IDEAS study was funded in an effort to gather this information for CMS and to provide evidence on the impact of amyloid PET testing. The scientific plan and protocol was developed by the study team and was approved by CMS.
The first aim of IDEAS study is to see if the results of an amyloid PET changed how clinicians managed these patients. The second aim is to see if the scan cuts down on subsequent health care utilization. This study is not about the accuracy of Alzheimer’s diagnosis—studies of the accuracy of amyloid PET have already been done. This study was done to see if this imaging scan has an impact on the patient.
What are amyloid plaques and how does this method detect them?
Amyloid plaques are deposits of protein “clumps” in the brain. Previous studies have shown that amyloid plaques are predictive of Alzheimer’s disease. However, there is controversy about whether the amyloid plaque formation causes Alzheimer’s. The amyloid plaque hypothesis was the basis for designing studies of drugs that attack the amyloid plaque. As of today, these drugs have failed to change patient outcomes, which calls into question the hypothesis of amyloid plaques being the causal agent. However, there is no question that amyloid plaques are predictive of Alzheimer’s.
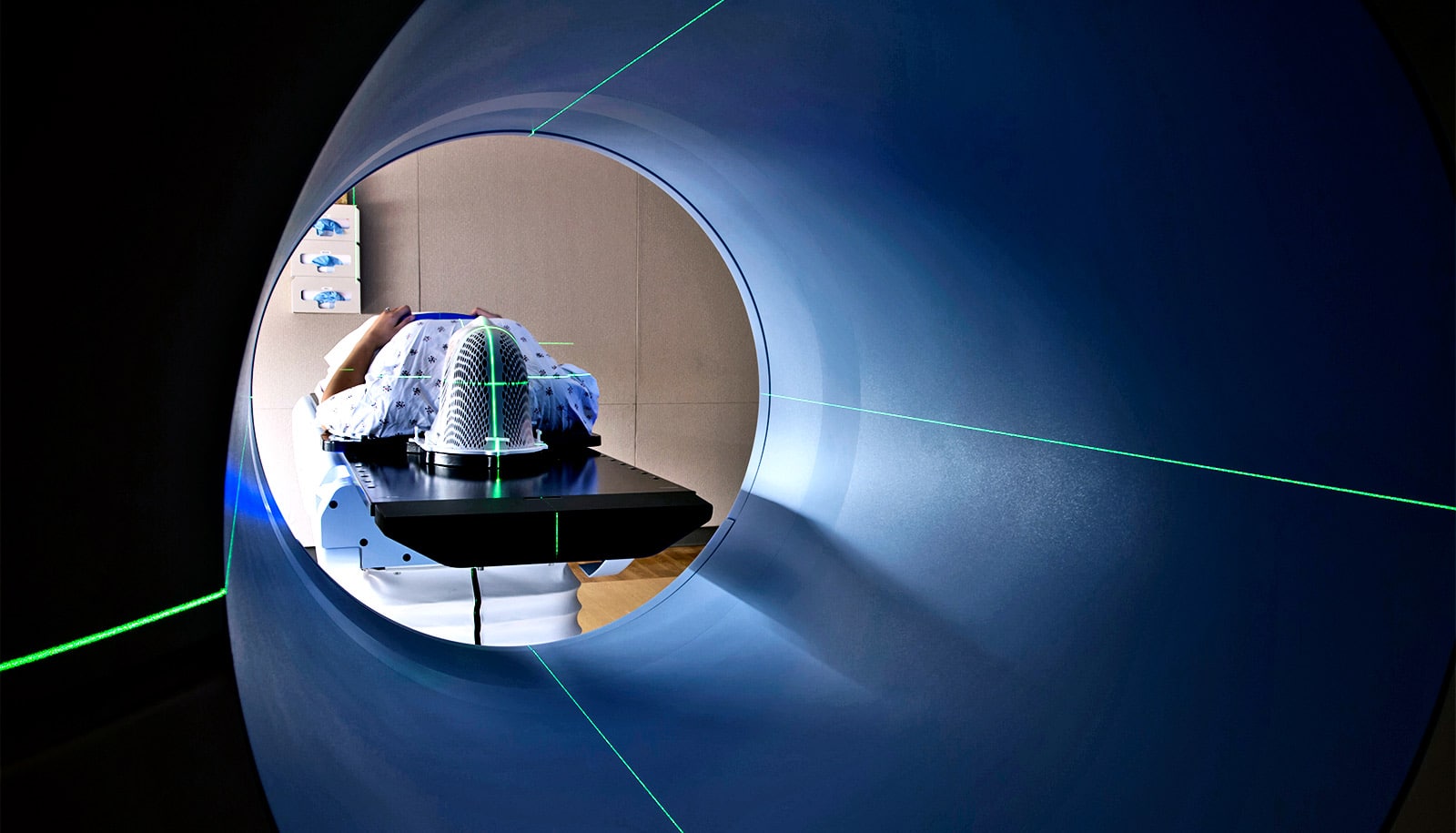
In general, a PET scan is a nuclear scan. The patient is injected with an agent marked with a radioactive substance that binds to the target of interest. The three agents we used in the study show a pattern when the amyloid plaque is there. Because PET scans are somewhat fuzzy, PET is combined with a CT—so you do the PET at the same time you take an X-ray computed tomography scan of the brain so you know where everything is. Previous studies have shown if this test is positive, you have an 80 to 90 percent chance of eventually getting Alzheimer’s.
What findings are being unveiled in this JAMA paper?
The first aim of the study, which is reported in this paper, answers the question of whether knowing the results of the PET scan affected the treatment decisions made by the patients’ physicians. This part of the study does not provide evidence of the longer-term, downstream consequences of the scan. Different types of dementias have overlapping symptoms making it difficult to tell them apart.
At the same time, it’s important not to treat people for conditions they don’t have. We saw that the PET scan produced substantial changes in clinician assessment of the disease and that clinicians changed their treatment of these patients.
If you asked me based on these findings, “Would you go do this scan?” I think I would. I want to know what is coming, and I would want to know this for my nearest and dearest as well. But we haven’t shown yet if we’ve made a real measurable difference in terms of patient outcomes. That’s the next paper. We have made a measurable difference in terms of how they are treated.
What was your role in the study?
For the IDEAS study, I and my colleagues here at [the Center for Statistical Sciences (CSS)] were deeply involved in formulating the scientific questions of the study.
A major question was how to evaluate the effectiveness of a diagnostic test when there are no therapeutic interventions for the disease itself, as it the case for Alzheimer’s. For somebody like me who has been thinking about diagnostic tests for a long time, it was an interesting challenge. Hence, there was a lot of brainstorming that needed to be done upfront about what is it that we’re going to evaluate, how might we evaluate it, and how will we organize the study to evaluate it?
Once the study got going, CCS monitored the data collection, and we are now doing the data analysis. One challenge in the analysis was to determine how to fit a complex set of actions and decisions into “change” and “no change” bins. That’s not trivial, despite the fact that the general criteria were defined in the study protocol. Clinicians live in a continuous, qualitative world. Another challenge was how to address patient dropout. Many people had a scan but didn’t come back for their 90-day follow-up visit, so we had to examine if the missing data biased the results, using a method called multiple imputation. In fact, addressing missing data was an important part of our analysis of factors that predict whether the amyloid PET scan is positive.
What are the next steps of the IDEAS study?
Right now we’re analyzing data for the second main question of the study, which is: Does the scan cut down on health care utilization? The idea here is that if somebody has an early warning from the PET scan, then can they can start planning changes in their living arrangements and behavior or somebody could monitor them more carefully. This may ultimately reduce hospitalizations and visits to the emergency room.
A lot of hospitalizations and other health care utilization for dementia patients come about because they stop being able to take care of themselves—people who are diabetic forget to check their blood sugar or to take heart medications, for example.
So we linked the data on people in the IDEAS study with their Medicare claims data. We now know how many times they visited the hospital and other health care utilization patterns for the year after the scan. We also went into the Medicare database and found matched controls for the participants in the study—people in the same area as the original participants with similar characteristics, but who did not receive a PET scan. We’re seeing if the IDEAS participants who had the amyloid PET scan had different amounts of health care utilization compared to similar Medicare beneficiaries who did not have the scan.
Additional researchers from the University of California, San Francisco; the Alzheimer’s Association; Virginia Commonwealth University; Washington University School of Medicine in St. Louis; the UC Davis School of Medicine; the Kaiser Permanente Division of Research; and the American College of Radiology contributed to the project.
Source: Brown University