Yale neuroscientist Vaughn R. Steele is spending the summer testing whether a treatment known as transcranial magnetic stimulation can help people with alcohol and opioid addiction.
Vaughn Steele is calling it his “summer of TMS.”
For weeks, Steele, an assistant professor of psychiatry at the Yale School of Medicine, and members of his lab have traveled to an addiction treatment center in Middletown, Connecticut, where they are administering a non-invasive treatment known as transcranial magnetic stimulation (TMS) to patients with treatment-resistant addictions.
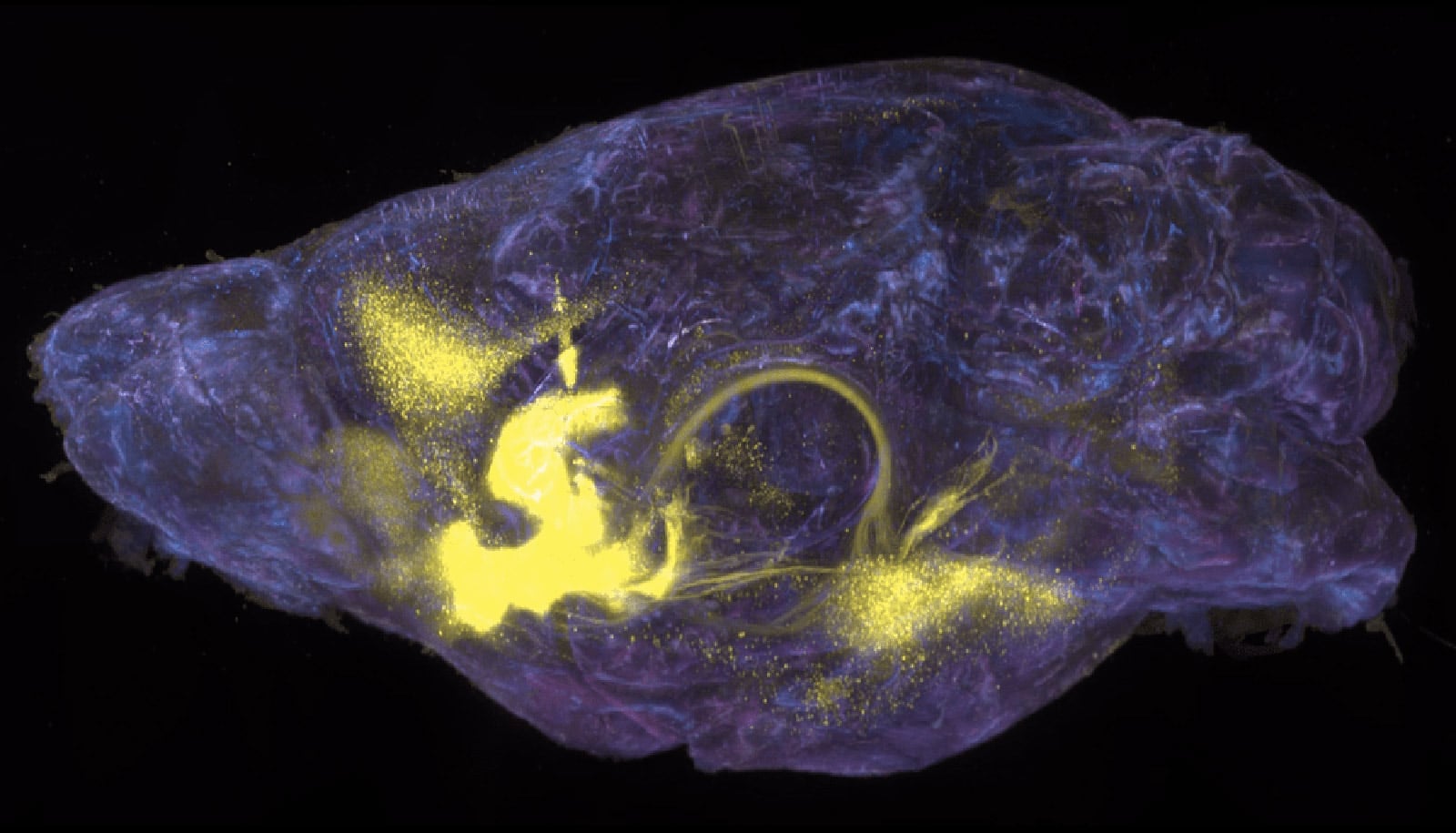
TMS uses electromagnetic pulses to stimulate specific areas of the brain, when treating depression and other psychiatric conditions. A coil placed near the patient’s head delivers pulses, with the hope of activating or inhibiting certain nerve cells. If successful, the treatment can disrupt addiction cravings and reduce future use.
A team led by Steele is administering TMS to roughly 40 participants who are struggling with either alcohol use disorder (AUD) or opioid use disorder (OUD). Participants are recruited just days after detox and are in the early recovery period of treatment at an in-patient facility. The study is the first of its kind to be administered during the early recovery stages, which are the most dangerous period for relapse, Steele says.
Treatments should wrap up by mid-August. Three months later, after patients have been discharged from the in-treatment facility, the researchers will conduct interviews to determine whether the participants have experienced a reduction in the amount and/or frequency of their alcohol or opioid use.
The hope is that resulting data will show TMS may help curb substance use during the early treatment stages for AUD and OUD. TMS has already proven effective in blunting nicotine craving in smoking cessation programs and in treating AUD in an out-patient protocol. Steele has had previous success using TMS to treat patients with cocaine use disorder.
“We’ll learn so much this summer about the feasibility and efficacy of TMS as an intervention in in-patient centers for OUD and AUD,” he says.
Here, Steele discusses the pressing need for new addiction treatments and the hope that TMS could hold for so many people:
How does TMS work in the brain of someone who has an addiction?
I hesitate to answer because we don’t exactly know what it does. But we do know that TMS uses electromagnetic pulses that generate an electric current in the brain, which then stimulates a person’s brain cells. With repeated stimulations, there’s some evidence that suggests it can change circuits in the brain or network connectivity in the brain, including addiction pathways.
I like the analogy of a gas pedal and a brake. The gas pedal fuels your craving to use drugs, and your brake—or your brain’s more disciplined, executive control functions—stop you from using drugs. These things are not balanced in people who are struggling with addiction. Sometimes people have too much craving and not enough brake or not quite enough brake. Then you can get out of control. The TMS styles that we’re using are trying to modulate one or both systems. The hope is that with TMS, we can modulate these circuits and change the behavior.
How did the idea for this summer project come about?
The general thrust of my research program is using TMS, or some sort of neuromodulation, to affect change in the brain in clinical populations. My primary focus is substance use disorders. I’ve been doing smaller TMS projects for about a decade, all leading up to the intervention this summer.
At Yale, I’ve done primarily single sessions of TMS as proof of concept to show that TMS, if put in the right place for the right sequence, can modify brain function, and behavior, in people with substance use disorders. The next step has always been trying to develop an intervention which would involve multiple sessions to try to change substance abuse behavior.
Why are new interventions and treatments such as TMS so critical now?
The treatments we have for alcohol and opiate addiction are too often insufficient to treat the underlying causes. The opioid overdose crisis we’re currently facing tells us that whatever we’re doing is not good enough. We need something else.
Opioid use disorder and alcohol use disorder are both immense public health issues, and they’re both terrible in different ways. Alcohol is a slower killer. You have more chronic issues than with opiates, where you can OD during a single use. In both cases, there are people suffering from these disorders who’ve tried multiple treatments, and they just haven’t worked.
What type of patients is TMS potentially targeting?
There’s a segment of the general population that gets addicted, and there’s a segment of that segment that is treatment resistant. A segment of that segment might respond to TMS. The goal isn’t to be able to cure addiction for everybody. But there’s a certain group of people that TMS could help. Honestly, addiction ruins your life. It takes over. If we can help give anybody their life back so that they’re not consumed with going to use their substance of choice, that would be a huge win. TMS is a tool that’s safe. It has very few side effects. It could potentially help a lot of people.
Are there other facilities currently using TMS to treat addiction?
There are several research trials out there, mostly for alcohol. There is an FDA indication [the process by which the US Food and Drug Administration defines the medical use of a potential intervention] for the use of TMS in smoking cessation, but it’s relatively new. But there isn’t anybody else doing things like what we’re doing here at Yale—targeting both alcohol and opioid use during early-stage treatment, in the hopes of gaining FDA indication to use TMS for addiction.
How is the protocol going?
We’ve been doing this every day since the middle of May, and it’s going way better than I anticipated. The Middletown staff has been fantastic and helped us recruit participants. People are excited to be in the study. There are times when we have too many participants for us to run, because we just don’t have enough staff.
We deliver the TMS treatment in two sessions, thirty minutes apart five days a week. TMS coils are placed on the forehead and on the side of the head to target different regions of the brain. We’re also comparing the effectiveness of two-minute sessions versus 10-minute sessions of treatment. There are different kinds of TMS, in terms of coil placement and length of delivery, and part of our inquiry is asking which type is most effective.
We’re well ahead of the amount of data I thought we would get. The goal was to get a handful of participants to show that this intervention might work and then publish the data. Ultimately, we want to pursue a grant idea that would allow us to expand to maybe a couple hundred participants, so we can get more definitive data that will get us closer to FDA indication.
We’re seeking funding from any interested donors, and my hope is to also have sufficient preliminary data to submit to the NIH [National Institutes of Health] in October.
What if the data aren’t as supportive of TMS as you’re hoping?
It’s all part of the process. Research is a long-term, cumulative undertaking. Each study either does or does not support a theory, which then directs the next phase of exploration. The summer of TMS data will shape our next steps in learning how to best utilize this technology to help as many people as we can.
The interview has been edited for length and clarity.
The study is funded by Yale’s psychiatry department and the Olin Neuropsychiatry Research Center at Hartford Hospital.
Source: Yale