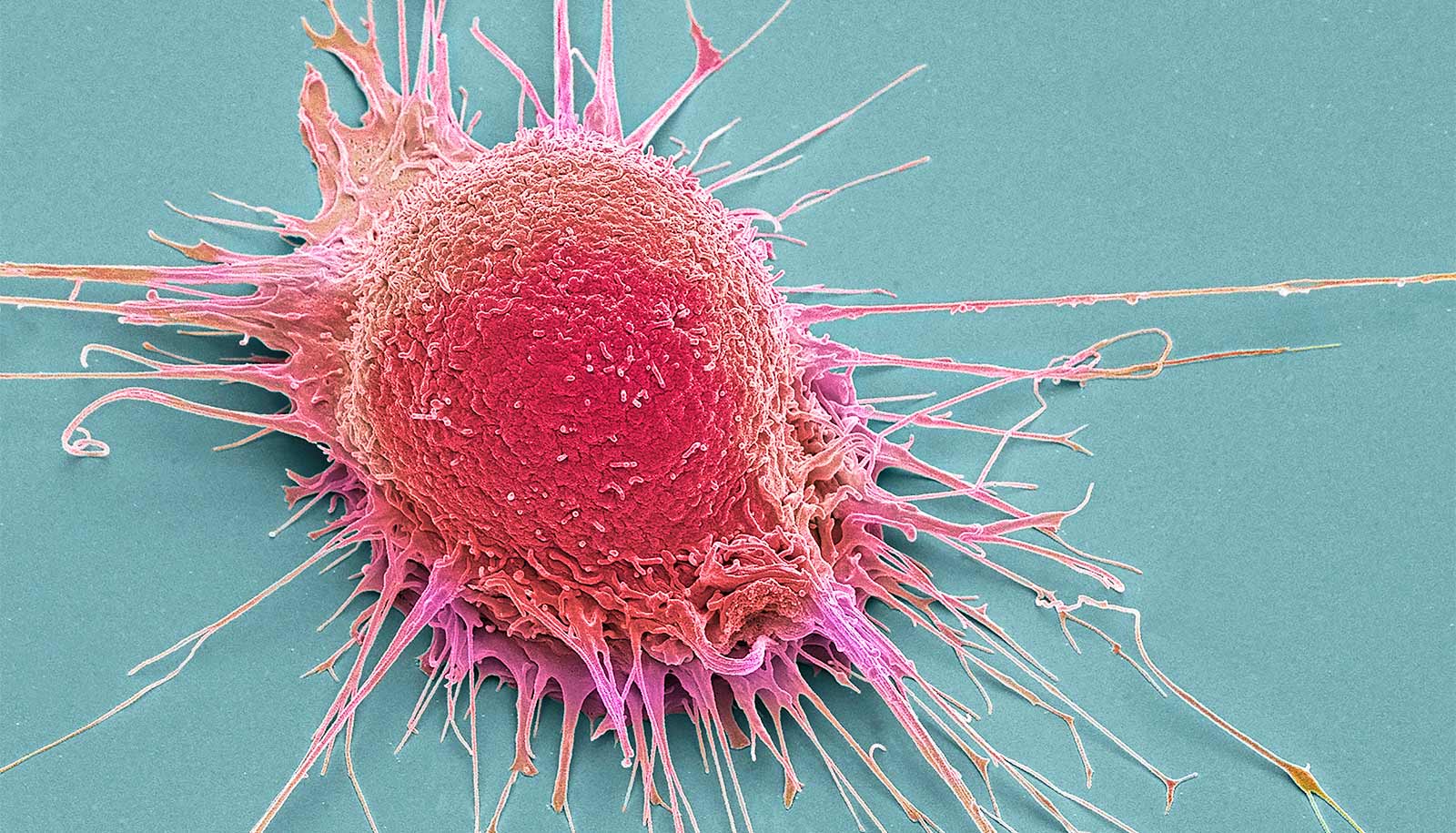
A new study finds that T cells, a type of white blood cell and an essential part of the immune system, are sufficient by themselves to establish and maintain an HIV infection in the brain.
“These results are paradigm changing,” says co-corresponding author J. Victor Garcia, professor of medicine at the University of North Carolina School of Medicine and a member of the UNC Institute for Global Health and Infectious Diseases, the UNC Center for AIDS Research, and the UNC Lineberger Comprehensive Cancer Center. “We have demonstrated for the first time that infection of the brain can be established and maintained by both human macrophages and T cells.”
“Despite effective suppression of HIV virus in the blood by antiretroviral therapy, we were still able to detect virus in the brain in more than 65% of the brains analyzed.”
The study, published in the Journal of Clinical Investigation, builds upon previous work by the same group of researchers, which found that the virus persists in HIV-infected macrophages and demonstrated the ability of tissue macrophages to support HIV replication in vivo in the total absence of human T cells. Macrophages are large white blood cells found in tissues throughout the body, including the liver, lung, bone marrow, and brain.
HIV/AIDs researchers long believed that myeloid cells are critical for HIV infection of the central nervous system. But more recent research indicates that HIV infection in cerebral spinal fluid can originate from both T cells and/or macrophages.
To directly address whether or not T cells contribute to the seeding and persistence of HIV infection in the brain, researchers in the laboratories of Angela Wahl and Garcia used a humanized T-cell only mouse model to determine whether or not myeloid cells are essential for HIV infection of the brain.
“In our studies we show that T cells are a major target of HIV infection in the brain, both in the presence and in the absence of macrophages,” says lead author Jenna B. Honeycutt, a postdoctoral research associate in the division of infectious diseases at UNC and the UNC Center for AIDS Research.
“In addition we describe a previously unknown phenomenon that occurs in the central nervous system rapidly after infection—specifically, a significant depletion of CD4 T cells within 1-2 weeks of infection in the brain.
“This has previously been reported for mucosal tissues, but has not been reported previously in the brain. We also report that the depletion of CD4+ T cells in the brain can be efficiently reversed by antiretroviral therapy,” says Honeycutt.
Marijuana chemical may keep HIV patients sharp
Another significant aspect of this work is that it establishes that the brain is not an immune-privileged site as previously thought, and that the possibility of a persistent reservoir for HIV in the brain has been severely underestimated.
“Despite effective suppression of HIV virus in the blood by antiretroviral therapy, we were still able to detect virus in the brain in more than 65 percent of the brains analyzed,” says Wahl, who is co-corresponding author of the study. “These results indicate that the brain may be an important reservoir for HIV in patients that should be targeted by HIV cure approaches. Future studies will be needed to determine if the virus that persists in the brain during ART is able to re-ignite the infection if ART is removed.”
The National Institute of Mental Health, the National Institute of Allergy and Infectious Diseases, UNC CFAR, the Natural Science Foundation of Guangdong Province, China, the UNC-South China STD Research Training Center, and CARE, a Martin Delaney Collaboratory of the NIAID, NINDS, NIDA, and NIMH of the National Institutes of Health, supported the work.