Researchers have zeroed in on what may be easily detectable markers of Parkinson’s disease.
The evidence is in the specific angles and sharpness of electrical waves in unfiltered raw data from scalp electroencephalograms of patients receiving treatment for the degenerative disease that slowly damages the central nervous system.
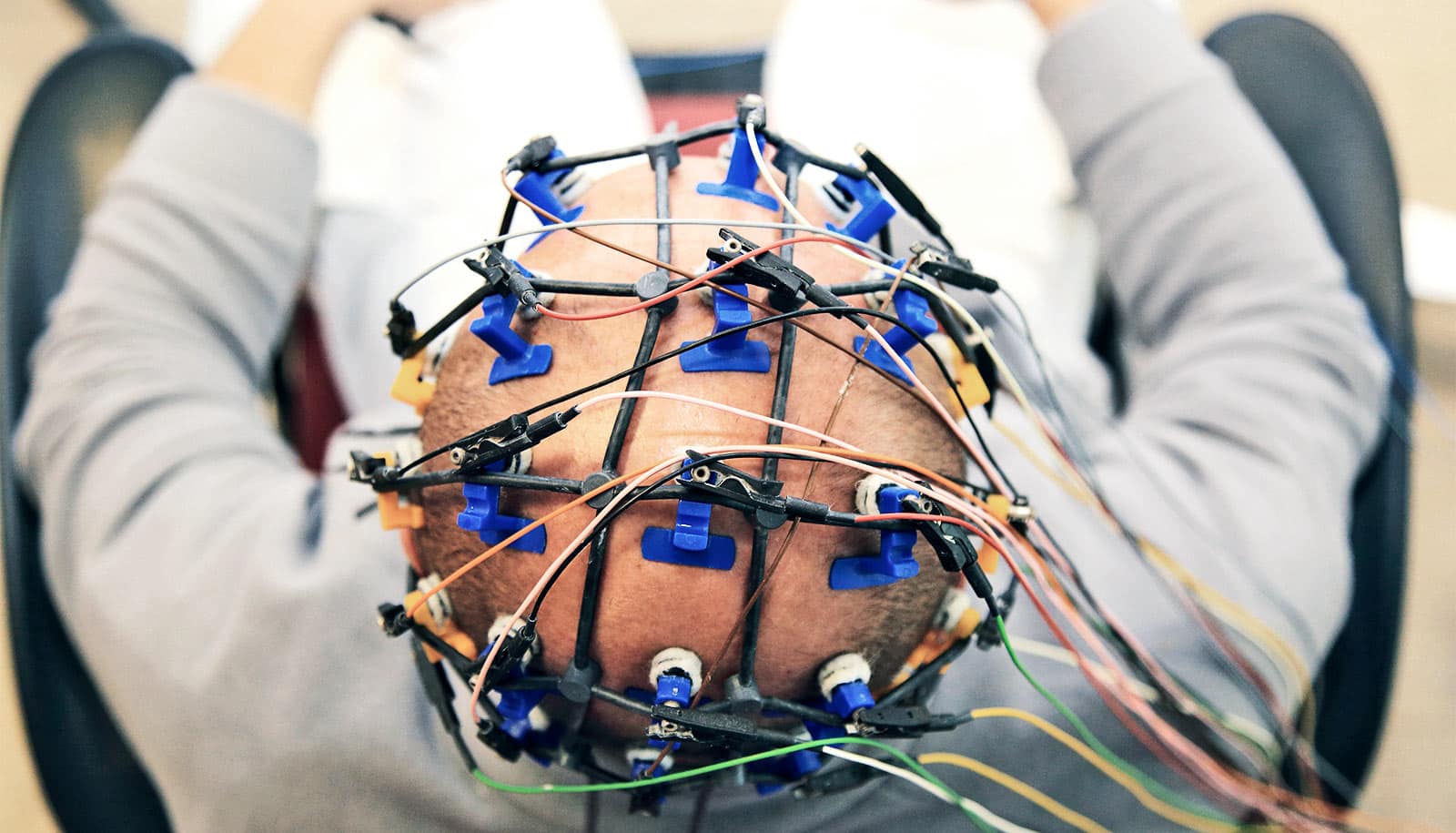
Medical facilities around the world use noninvasive scalp EEG, in which electrodes briefly placed on the head measure brain waves. Harnessing the relatively inexpensive technology could aid in both the diagnosis of Parkinson’s disease and fine-tune therapeutic treatments for Parkinson’s and other motor disorders, says Nicole Swann, a professor in the human physiology department at the University of Oregon.
“Using this safe and affordable way to measure and quantify brain activity, we were able to distinguish differences between Parkinson’s patients who were on and off medications and in comparisons with healthy people,” says Swann.
The angle of the waves
In 2017, coauthor Scott Cole, then a doctoral student at the University of California, San Diego, had noticed that Parkinson’s patients appeared to have sharp brain waves in invasive brain recordings acquired during neurosurgery, suggesting a new look was warranted.
The new study, Swann says, shows that similar patterns are evident in scalp EEG recordings—an affordable and safe method which doctors can use on anyone—extending the translational power of the previous work.
Previous efforts to detect Parkinson’s disease with EEG have been inconsistent, she says, because researchers have modeled brain signals as sine waves, which are beta waves filtered to round the waves and show the overall power of periodic oscillations. The current work uses a new analytic approach.
“The raw signals go up and down like sine waves but with more asymmetry,” Swann says. “The steepness—the slant—turns out to be important in Parkinson’s patients. This was easily detectable in the patients who are off medication.”
When the peak is sharper at the top of the wave than in the trough, or low part of the oscillation, it is indicative of patients who are off their medications, she says.
The initial diagnosis of Parkinson’s disease now relies on a neurologist’s assessment of patients as they complete a series of body-movement tasks. Such subjective testing, however, can lead to misdiagnosis.
“We don’t know yet whether this approach will be better, but it could provide easily obtained brain measurements that would be helpful and possibly used in tandem with clinical observations and other EEG measurements,” Swann says.
Real time treatment changes?
Current treatments for Parkinson’s disease involve surgery to permanently implant an electric stimulator and/or a drug-based approach where finding the best dosage is difficult and often results in frustrating cycling of effectiveness, says coauthor Bradley Voytek, a neuroscientist at the UC San Diego.
In a large, upcoming follow-up study, Swann says she hopes to combine scalp EEG measurements with detailed medical histories of patients, along with self-reports of how each person is feeling on testing days. Eventually, she hopes the approach could help detect changes in the disease in individuals over time.
Finding such measures of the course of the disease in real time, Voytek says, could lead to quick treatment adjustments.
“In the case of an invasive brain stimulator, this might mean only applying electric stimulation when it’s needed,” he says. “In the case of pharmacology, it would mean adjusting a drug’s dose much like continuous glucose monitoring done by an implant can signal a pump to adjust insulin levels as needed.”
Ideally, Swann says, if the approach proves to provide robust information, Parkinson’s patients could get EEG testing remotely by wearing a hat fitted with electrodes. The data could then go to their doctor to help avoid frequent trips to a neurologist for patients for whom travel may be a barrier to treatment.
The findings appear in eNeuro.
Source: University of Oregon