A new paper could open the door to better understanding and potentially, better self-care, for people with multiple sclerosis.
For people with multiple sclerosis (MS), hearing a doctor tell them they are experiencing brain atrophy—an important, predictive biomarker of MS disease progression—can trigger debilitating fear and anxiety.
The new paper, published in the Journal of Neurology, describes how clinicians can best communicate highly sensitive and technical information about an individual’s MS disease progression.
“Each group involved in this publication—researchers, providers, and especially patients—has contributed a valuable perspective to the goal of better communication about this complex disease,” says corresponding author Robert Zivadinov, professor of neurology in the Jacobs School of Medicine and Biomedical Sciences at the University at Buffalo and director of the Buffalo Neuroimaging Analysis Center (BNAC). Zivadinov also directs the Center for Biomedical Imaging in UB’s Clinical and Translational Science Institute.
The research grew out of a collaboration between BNAC researchers and the center’s Advisory Council, whose mission is to provide a patient’s perspective to the center’s team of neuroimaging researchers.
Getting specific
“Our goal is to minimize misunderstanding and apprehension about brain atrophy, also known as brain volume loss, which can seem so devastating it can affect patients akin to how a cancer diagnosis would,” says Penny Pennington, a lead author of the paper and co-chair of the Advisory Council’s Research and Education Committee. She has lived with MS for over 40 years.
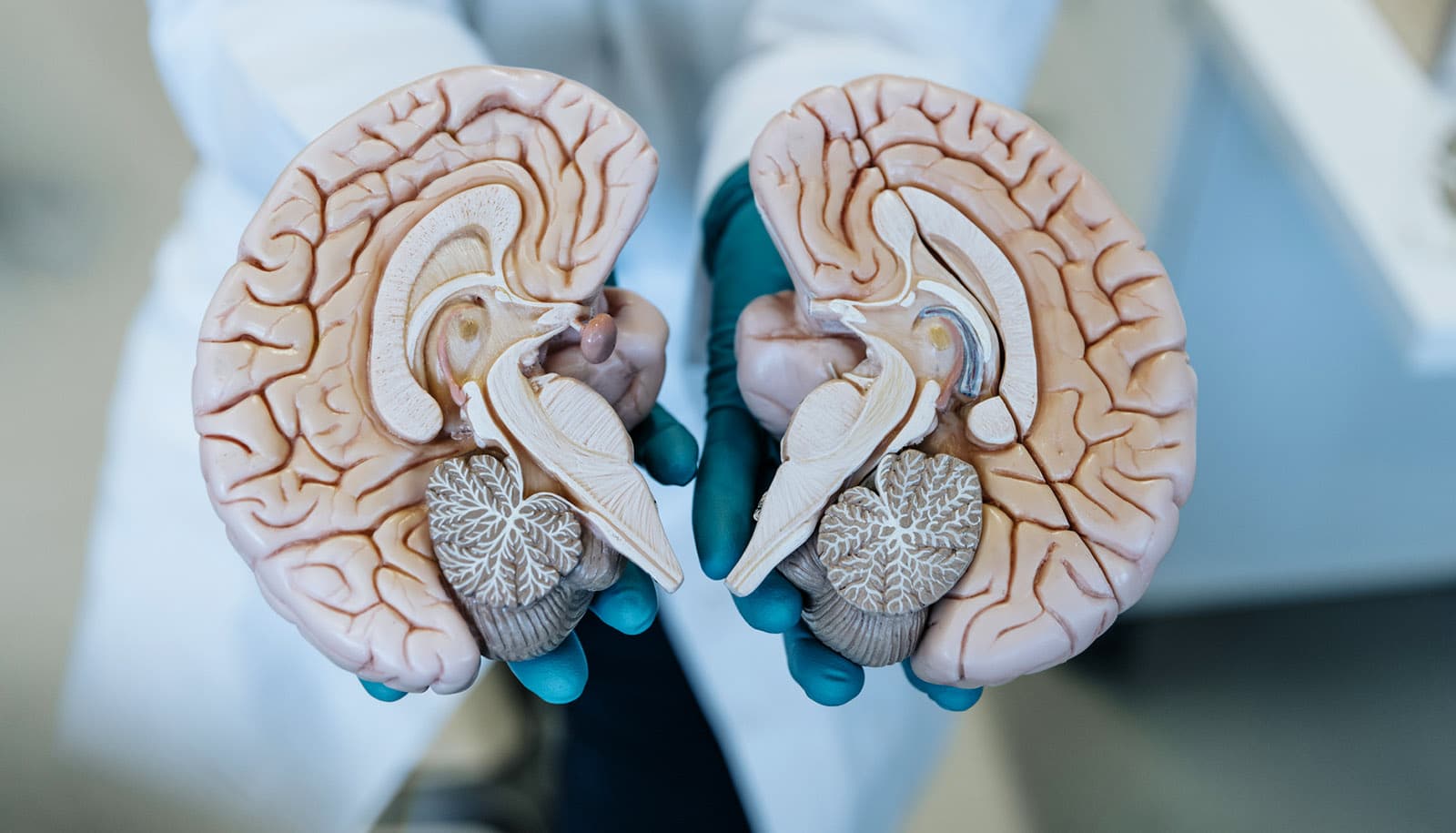
In people with MS, small increments of neurodegeneration and resulting brain atrophy (brain volume loss), as measured by magnetic resonance imaging (MRI) are becoming increasingly better understood as important prognostic biomarkers that can predict patients’ progressive disability.
Yet, based on their experience with patients’ reactions, there is evidence that some clinicians would prefer to avoid the discussion of atrophy altogether.
The authors found that general statements by clinicians, such as “what the research shows” for the larger population of people with MS are often not helpful and that there is a need to be technically specific.
The paper presents a model for how the medical community can assess and integrate the views of patients, medical providers, and researchers to arrive at guidelines to help ensure that patients are given vital information about their disease progression.
While the paper deals solely with MS, it could pave the way for patient advisors with other diseases to tackle similarly challenging communication issues.
13 recommendations
“Sometimes hard-to-hear or hard-to-communicate information can be essential in convincing patients to pursue or adhere to behavior changes or treatment protocols that can materially improve their quality of life,” says Pennington. “Yet too much or too little information, or a muddled, hurried explanation in a doctor’s office can have the opposite of its intended effect on patient care.”
This reality, coupled with the dramatic increase in the availability of online medical information, can contribute to an unavoidable dilemma for providers and widely disparate views about the best way to communicate with patients, she adds.
“By listening to the perspectives and achieving important consensus among the three critical types of players—patients, clinicians, and researchers,” says Pennington, “we were able to arrive at 13 tangible recommendations for clinicians. There is a meaningful opportunity now for the MS community to come together to produce the necessary informative materials and standardize patient interaction practices.”
Over the course of two years, three subcommittees consisting of researchers, providers, and patients were organized. They subsequently conducted workshops and surveys to gather relevant data on current specialty provider practices for discussing MRI findings as well as patient perceptions regarding MRI findings. Thirteen practicing MS specialists from six academic and non-academic MS centers in the US participated in the survey along with 26 randomly selected patients seen at the University at Buffalo’s Jacobs MS Center for Treatment and Research.
Recommendations include a need to provide basic information on brain anatomy and neurodegeneration and cautions about the state of the science and MRI technology. The paper includes a patient discussion guide as a resource for providers. Especially important, the authors say, is the need to explain how an individual patient’s atrophy measurements compare with those associated with normal aging.
It is recommended that providers discuss with patients how inflammation and neurodegeneration in the brain is measured and how they contribute to brain atrophy in MS.
Providers are urged to emphasize that MS is clinically, not radiologically, diagnosed and that treatment decisions should not be based rigidly on MRI findings alone. Communicating to people with MS the benefits of both physical and mental exercise to help build brain reserve that can slow or reverse the neurodegeneration that leads to brain atrophy is also key.
The authors found that the more a patient understands the role of brain atrophy and other MRI metrics, the more accepting they may be of the value of MS therapies.
“It is extremely helpful to researchers to see how they can contribute to resolving the dilemma that now confounds so many clinicians and that results in so much unnecessary anxiety and confusion experienced by countless patients,” says Zivadinov.
Additional coauthors are from the University at Buffalo, Wayne State University, the University of Nebraska Medical Center, the Oklahoma Medical Research Foundation, Negroski Neurology, and the Michigan Institute for Neurological Disorders.
Source: University at Buffalo