It’s only a matter of time before scientists will be able to take cells from a person’s mouth or skin and, using a process called in vitro gametogenesis, turn those cells into human eggs or sperm.
Which means, says Eli Y. Adashi, a professor of medical science at Brown University’s Warren Alpert Medical School, that those eggs and sperm can then be fertilized to create an embryo—all in a lab.
In fact, it’s only a matter of time before scientists will be able to use a person’s cheek cell to custom-create any kind of cell, Adashi says.
“Using induced pluripotent stem cells, you could make a neural cell that would perhaps help a paralyzed person walk, or a cell that you could implant in the brain of a patient with Parkinson’s disease and, in theory, cure Parkinson’s disease,” Adashi says. “It’s essentially a replacement technology that allows you to make new spare parts when the original parts are not working.”
The possibilities are endless—and so, too, are the ramifications. This, Adashi says, is what motivated the National Academies of Sciences, Engineering and Medicine to host a multi-day workshop discussing scientific, ethical, and regulatory implications of in vitro-derived human reproductive cells.
“The National Academy of Medicine recognizes the potential and implications of IVG, and concluded that this was a topic worthy of attention at this time, while realizing full well that it’s not yet at the stage of application,” Adashi says.
Here, Adashi discusses the resulting report, and his thoughts about the potential of using this advanced technology to create human sperm and eggs:
What is the state of the science for in vitro gametogenesis—or IVG?
The work on IVG dates back to about 2009. In 2013, I had an opportunity to be in Japan, and I booked a flight to Kyoto to meet the two scientists who were really making this happen, Katsuhiko Hayashi and Mitinori Saitou. They had been able to take skin cells from a mouse’s tail, reprogram them into what we call induced pluripotent stem cells (or iPSCs), and then turn those stem cells into egg cells.
I made a point of meeting with them and I spent an hour or two with them in their laboratory and got a personal primer, if you will.
These Japanese investigators, and now some other investigators around the world, have since been able to take these iPSCs that can become anything and make an egg or sperm in the rodent. They then use those egg and sperm cells to fertilize the appropriate opposite gamete to give rise to an embryo that is then implanted in foster mothers, who then give birth to pups. Some of those pups were also able to reproduce.
IVG has so far only been accomplished in rodents. We’re nowhere near human application. It will be probably a good few years, if not a decade or two, before we get there. As we speak today, it’s not even a theoretical possibility in the sense that there is no paper in the literature that has documented IVG in the human from A to Z. And even if we get there, we will still need to have this technology approved in the United States by the Food and Drug Administration before it could ever be applied in the clinic.
How would IVG affect IVF as we know it today?
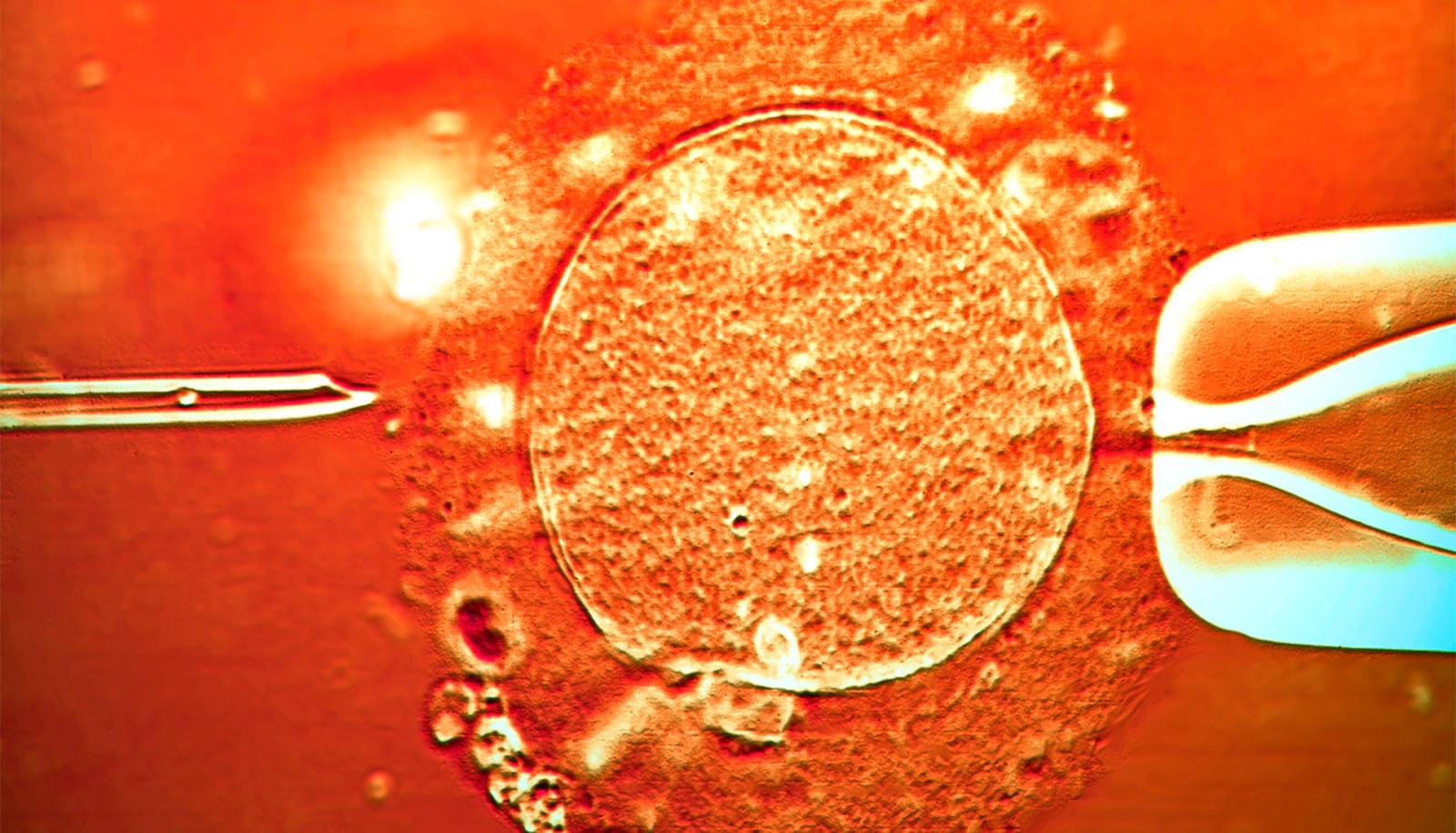
In the procedure of in vitro fertilization, or IVF, a woman requires hormonal treatments via injection to stimulate egg production. The injections are administered for several weeks, and then the woman is subjected to a minor but not-insignificant surgical procedure in the clinic to retrieve the eggs. The eggs are placed in a dish and fertilized. The resulting embryos are transferred into the womb in the hope that a pregnancy will ensue.
IVG will essentially simplify IVF for women. They will not have to get hormonal injections, and they will not need a surgical procedure. Instead, the women in question would simply provide a cell from the inside of their cheek or from their skin. The IVF process would thus become more of a laboratory procedure than a clinical one.
The only procedure the woman in question would have to undergo is the placement of an embryo into the uterus. That cannot be avoided, of course, until such time that we can grow embryos outside the womb. This, too, is under discussion, in a separate area of science, even as we speak.
The report summarizes a discussion on the social, ethical, and legal implications of IVG. Can you share some of the big takeaways?
In the normal IVF process, you retrieve 10, maybe 14 eggs. But in IVG, you can create essentially an unlimited number of eggs. There is the potential to create many more human embryos, for research or clinical use, than current assisted reproductive technologies. Discussions and oversight will be required to address the implications of increased embryo selection and the challenge of embryo disposition.
Another possibility that was considered is the case of women who, for one reason or another, are born without ovaries or are born with ovaries that are non-functional. People with Turner Syndrome, for example, are born with ovaries, but their chromosomal makeup does not permit them to create normal eggs. In theory, you could provide these women with eggs, but you would also have to do some genetic engineering to address their genetic makeup. And the idea that we could do this for women without ovaries is now beginning to take off in all kinds of unexpected directions.
For example, for the first time in human history, it may become possible for same-sex couples to be the genetic parents of children. Nature Magazine in March reported a technology that involved, among other things, IVG used in the creation of a rodent with two so-called fathers.
So we can imagine a situation where two males could actually become the genetic parents of a child, although they would still require a surrogate to carry the pregnancy. But in the case of two women who also are unable to become the genetic parents of an offspring, that could also become possible. And by the nature of their biology, one of them could carry the fetus. The applications of IVG are already taking off in directions that would have been thought of as unworkable as recently as five or 10 years ago.
What do you hope will be the impact of the report?
It’s all about disseminating knowledge and insights. The National Academy of Medicine accomplished several things: It put together the first significant multidisciplinary meeting that dealt with the idea of IVG. Secondly, the academy lent its weight to the need for scientific and social discussions about this concept now. And thirdly, they exposed the concept to a much larger number of people that otherwise would have never heard of IVG, and would have been surprised and unprepared when it finally becomes a reality.
I work in the reproductive arena, and while I have given lectures on the subject in multiple contexts, I’m cognizant of the fact that many of my colleagues are not familiar with IVG. It’s not taught in medical school; it’s not widely taught in residency or fellowship training programs. And so young physicians on the whole still are not quite familiar with this concept.
I think that prior to this time, it was really up to people who read the literature and saw the potential and gave lectures and so forth to disseminate insights. But when you have an organization like the National Academy of Medicine throw its weight behind the need to discuss something like this, it’s a sea change. It really takes a concept and puts it front and center and turns it from a theoretical preoccupation that is happening in some labs in a different country to something that will, at some point, need to be reckoned with by all medical providers across multiple fields.
This meeting was dedicated to reproduction, but if one listened carefully, one could deduce what we’ve discussed here, which is that this technology could be applied to other fields of medicine. And as such, this makes it a very powerful technology. It’s medicine at its very core.
While the technology isn’t there yet, it was time for the scientific public and the public at large to get a sense of the possible.
Source: Brown University