An implant containing cartilage derived from stem cells reduced pain and restored hip joint function to baseline levels in a study of dogs with symptoms of moderate osteoarthritis.
The study could be a significant first step toward preventative, less invasive joint resurfacing in dogs and humans, according to a new study.
“We were thrilled that the implant was so effective at restoring the activity levels of the animals.”
In humans—and dogs—a single, millimeter-thick layer of cartilage can mean the difference between an active lifestyle or painful osteoarthritis. That tiny cap of cartilage is what protects joint surfaces and allows the bones to glide over one another smoothly. Age or joint injury can cause the cartilage to degrade, leading to osteoarthritis and progressive joint pain.
“One of the holy grails of orthopedics is to replace cartilage, but there hasn’t been an effective way to do it,” says Duncan Lascelles, professor of surgery and translational pain research and management at North Carolina State University and co-corresponding author of the research in Science Advances.
“Most of the focus is on replacing or restoring the cartilage surface with artificial materials, but regenerating cartilage isn’t possible right now. And many of the artificial products in use don’t integrate with the body.”
Farshid Guilak, professor of orthopedic surgery at Washington University in St. Louis and Shriners Hospitals for Children, along with Bradley Estes and Frank Moutos, founded Cytex Therapeutics to develop an implant that could replace damaged or missing cartilage.
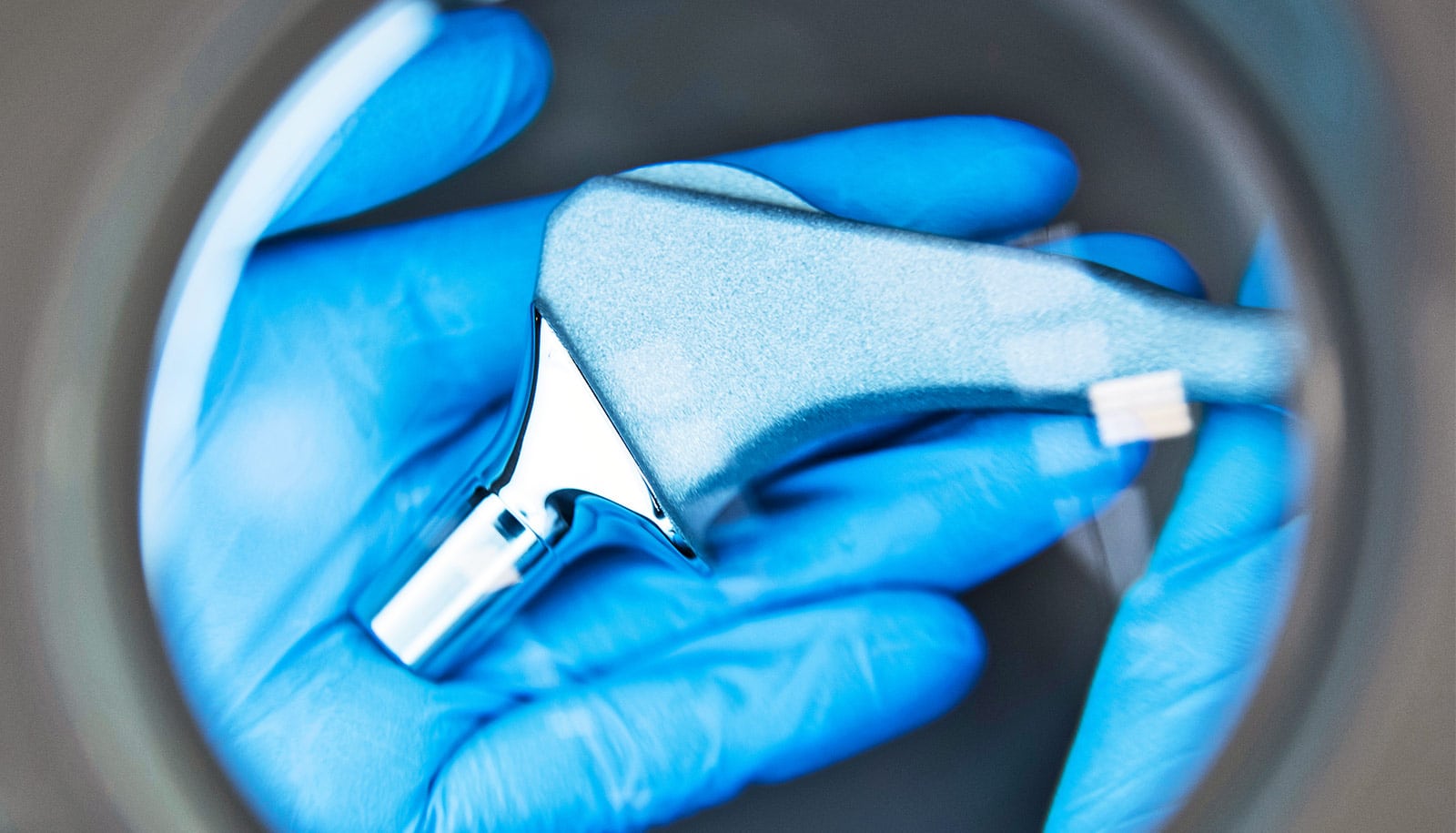
The implant is made using a combination of manufacturing techniques that result in a part textile, part 3D-printed structure, which can be seeded with the patient’s own stem cells.
“Combining 3D printing with advanced textiles enabled us to engineer an implant that mimics the function of native, healthy tissues in the joint from day one after implantation,” Estes says. “We also designed it to dissolve over time so that, ultimately, joint function is transferred back to the patient’s own tissues during the healing process.”
The researchers designed a study to test the implant for resurfacing joints in dogs, a critical step in translating this technology into use for both canine and human patients.
The researchers allowed cartilage to grow on the implant for several weeks before surgery. Then the implant was placed into the damaged area of the hip’s ball joint. Over time, the implant dissolved, ultimately leaving only the patient’s own natural tissue in the repaired hip joint.
Researchers divided the dogs in the study into two groups—one which received the implant, and a control group which did not. Lascelles, Masataka Enomoto, an NC State research associate, and colleagues performed the surgeries and measured subsequent joint pain and function in both groups.
Four months post-surgery, the group that received the cartilage implant had returned to baseline levels for both function and pain, while the control group never improved. The researchers also saw evidence that the implant had successfully integrated into the hip joints, effectively resurfacing them.
“What we saw is that with the implant these dogs were doing as well as or better than they would be after a total joint replacement,” Lascelles says.
“We were thrilled that the implant was so effective at restoring the activity levels of the animals,” Estes says. “After all, this is why patients go see their physicians—they want to be able to play tennis, play with their kids, and, in general, re-engage in a pain-free active lifestyle that had been taken away by arthritis.”
Lascelles hopes that the implant will address some of the issues involved with total joint replacements in young and active patients.
“There are significant drawbacks to total joint replacements in the young patient,” Lascelles says. “The surgery is more complicated, and the artificial joints are only good for a particular number of years until they must be replaced, often with poorer results each time.
“This procedure is less invasive, and the implant uses the body’s own cells and integrates into the damaged area with little danger of rejection. We believe that it is an early intervention that could be a major advance in postponing joint replacements for dogs and hopefully one day for humans.”
Shriners Hospitals for Children, the Arthritis Foundation, the Nancy Taylor Foundation for Chronic Diseases, and the National Institutes of Health funded the work.
Cytex Therapeutics has licensed the implant technology. Enomoto and Estes are co-first authors of the paper. Additional researchers from the Medical College of Wisconsin and Purdue University contributed to the work.
Source: NC State