Soft microparticle sensors can monitor oxygen levels in hydrogels that serve as scaffolds for growing tissues, researchers report.
When scientists place hydrogels in development at an injury site, they encourage the growth of new muscle, cartilage or, perhaps someday, entire organs because they contain live cells. Ideally, the hydrogel attracts blood vessels that infuse the material and bring nourishment to the cells.
Jane Grande-Allen, a professor of bioengineering and chair of the bioengineering department at Rice University, and her team designed fluorescent particles to report on oxygen levels inside gels. Their work appears in the journal ACS Biomaterials Science and Engineering.
“We’ve been collaborating with investigators in intestinal mechanobiology and wanted a straightforward way to tell what level of oxygen we had throughout our 3D tissue cultures,” Grande-Allen says. “Where we intend a specific level of oxygen, we want to be sure that’s what the cells are getting.
“There are multiple ways of doing this,” she says. “We can have computational models, but we’d have to make several assumptions about the way oxygen permeates the culture medium and 3D scaffold material. A better way is to measure it directly, so that was our goal.”
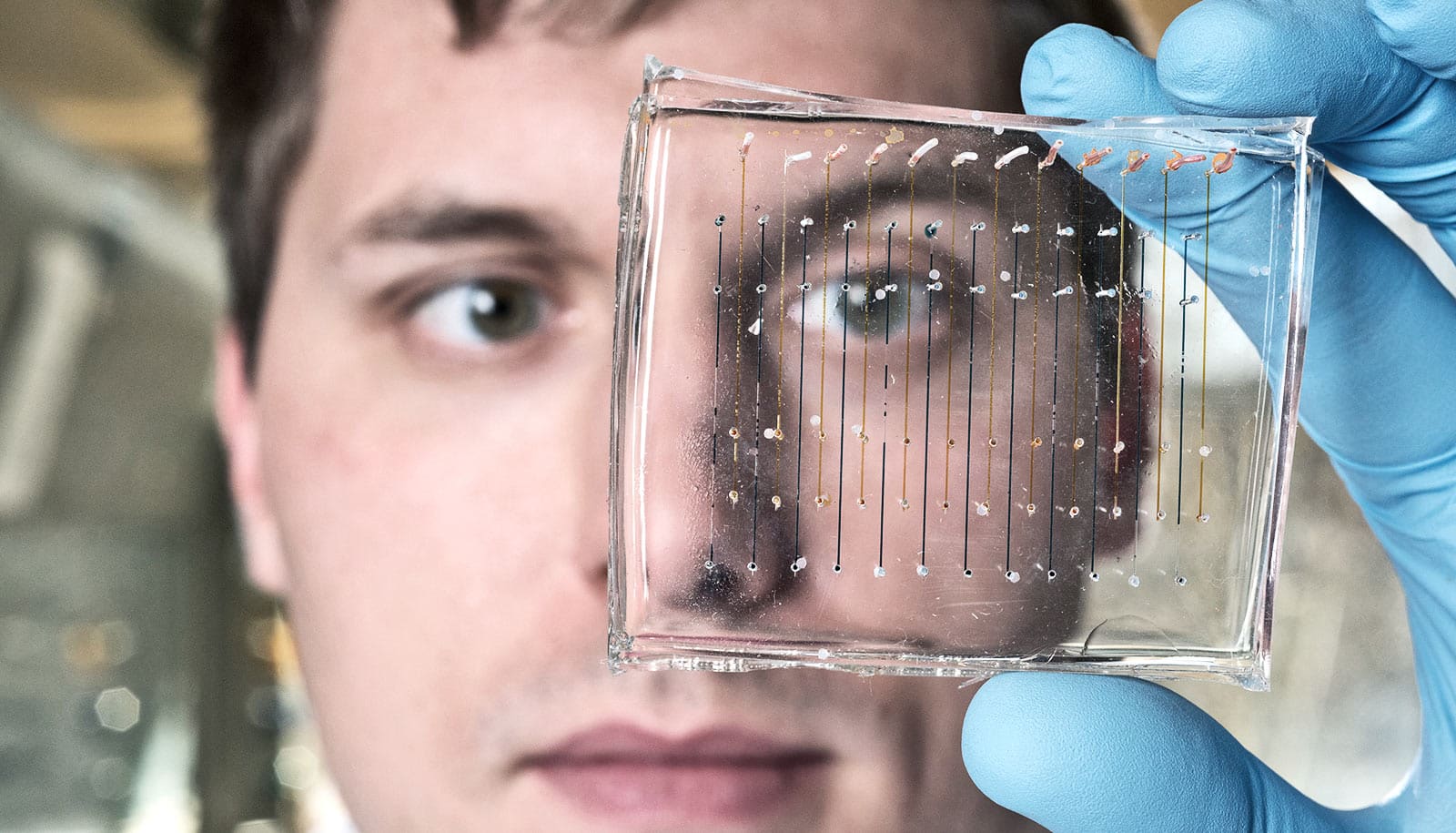
Lead author Reid Wilson, an MD/PhD student at Rice and Baylor College of Medicine, developed soft microparticles that that incorporate an oxygen-triggered fluorescent molecule based on palladium and a reference fluorophore.
Wilson went through several iterations of dye combinations and concentrations to develop those microparticles.
“The problem with using oxygen-responsive fluorophores in three-dimensional cultures is their signal isn’t bright enough to measure reliably,” he says. “So we loaded the microparticles with high concentrations of dye, which allowed more reproducible measurements of the oxygen concentration.”
The particles can be suspended in hydrogel along with living cells, and tests show they are not toxic to those cells. Researchers can read the signals from the fluorescent components at their individual wavelengths, but their power lies in combining the response from both, which gives clinicians the ability to measure oxygen content as far as 2 millimeters (less than one tenth of an inch) into tissues.
“That’s small, but oxygen diffusion limits are usually tiny,” Grande-Allen says. “Some cells are quite close to a blood supply, with a high oxygen level brought in by blood cells with hemoglobin. But some bacteria in the microbiome are normally anaerobic and survive better without oxygen.”
Grande-Allen says the particles aren’t susceptible to photobleaching (fading) when illuminated at the proper wavelength, nor did they sink out of the hydrogel, as larger fluorescent particles were prone to do, even after a year in storage.
She notes that tissues like cartilage and certain types of diseased heart valves don’t have vascular networks, yet their cells thrive. “I’ve always wondered how these cells get nourishment and what they need to survive,” she says. “With oxygen-sensing microparticles and other techniques we use in my lab to stretch living and engineered materials, we can start to work toward answering these questions.”
The National Institute of Allergy and Infectious Disease and the National Institute of Diabetes and Digestive and Kidney Diseases supported the research.
Source: Rice University