Why do some babies react to perceived danger more than others? According to new research, part of the answer may be found in a surprising place: an infant’s gut bacteria.
The human digestive system is home to a vast community of microorganisms known as the gut microbiome. Researchers discovered that the gut microbiome was different in infants with strong fear responses and infants with milder reactions.
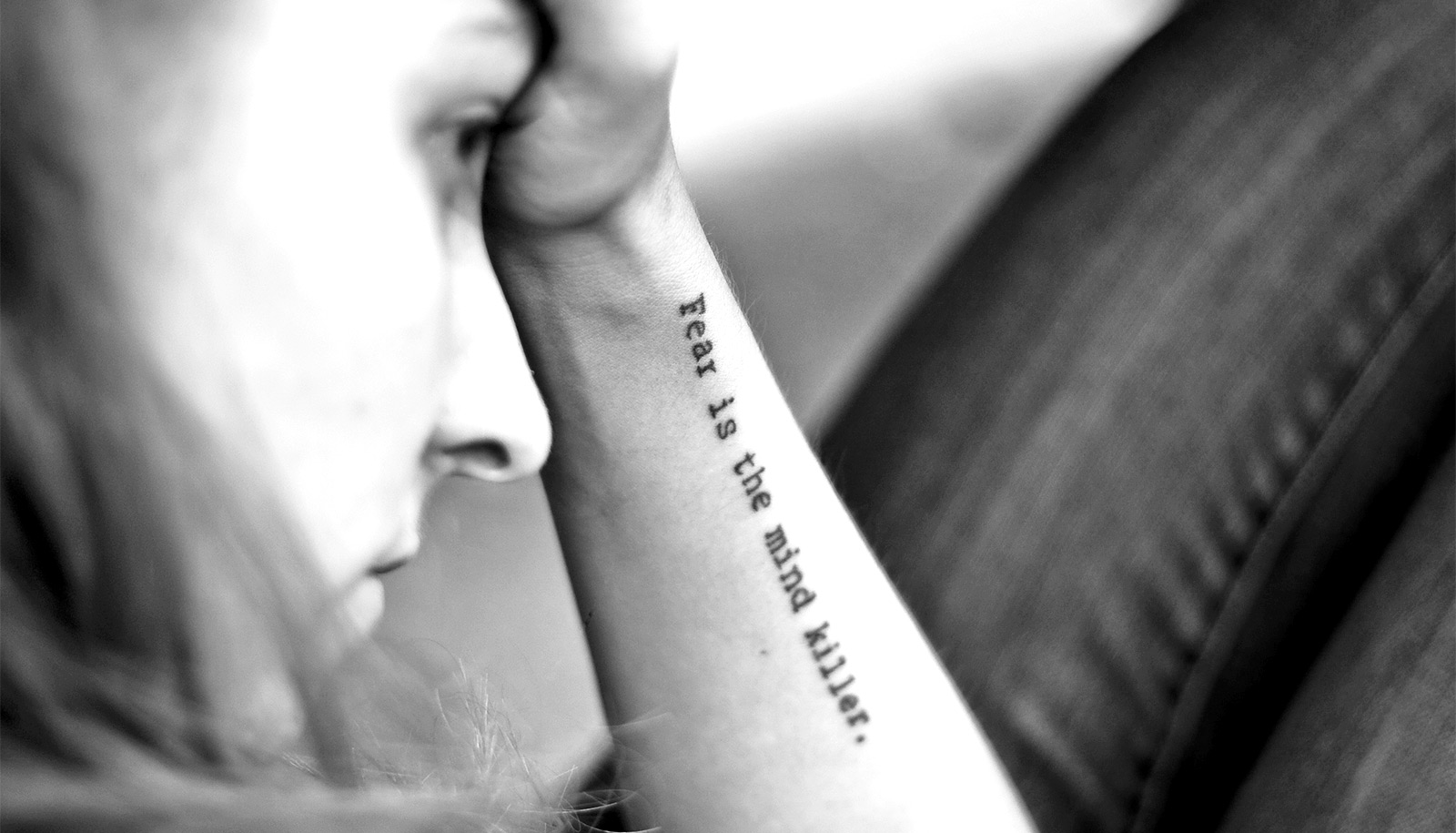
These fear responses—how someone reacts to a scary situation—in early life can be indicators of future mental health. And there is growing evidence tying neurological well-being to the microbiome in the gut.
The new findings suggest that the gut microbiome could one day provide researchers and physicians with a new tool to monitor and support healthy neurological development.
“This early developmental period is a time of tremendous opportunity for promoting healthy brain development,” says Rebecca Knickmeyer, leader of the new study in the journal Nature Communications. “The microbiome is an exciting new target that can be potentially used for that.”
Studies of this connection and its role in fear response in animals led Knickmeyer, an associate professor in Michigan State University’s College of Human Medicine’s pediatrics and human development department, and her team to look for something similar in humans. And studying how humans, especially young children, handle fear is important because it can help forecast mental health in some cases.
“Fear reactions are a normal part of child development. Children should be aware of threats in their environment and be ready to respond to them” says Knickmeyer, who also works in the Institute for Quantitative Health Science and Engineering, or IQ. “But if they can’t dampen that response when they’re safe, they may be at heightened risk to develop anxiety and depression later on in life.”
On the other end of the response spectrum, children with exceptionally muted fear responses may go on to develop callous, unemotional traits associated with antisocial behavior, Knickmeyer says.
To determine whether the gut microbiome was connected to fear response in humans, Knickmeyer and her coworkers designed a pilot study with about 30 infants. The researchers selected the cohort carefully to keep as many factors impacting the gut microbiome as consistent as possible. For example, all of the children were breastfed and none was on antibiotics.
The researchers then characterized the children’s microbiome by analyzing stool samples and assessed a child’s fear response using a simple test: observing how a child reacted to someone entering the room while wearing a Halloween mask.
“We really wanted the experience to be enjoyable for both the kids and their parents. The parents were there the whole time and they could jump in whenever they wanted,” Knickmeyer says. “These are really the kinds of experiences infants would have in their everyday lives.”
Compiling all the data, the researchers saw significant associations between specific features of the gut microbiome and the strength of infant fear responses.
For example, children with uneven microbiomes at 1 month of age were more fearful at 1 year of age. Uneven microbiomes are dominated by a small set of bacteria, whereas even microbiomes are more balanced.
The researchers also discovered that the content of the microbial community at 1 year of age related to fear responses. Compared with less fearful children, infants with heightened responses had more of some types of bacteria and less of others.
The team, however, did not observe a connection between the children’s gut microbiome and how the children reacted to strangers who weren’t wearing masks. Knickmeyer says this is likely due to the different parts of the brain involved with processing potentially frightening situations.
“With strangers, there is a social element. So children may have a social wariness, but they don’t see strangers as immediate threats,” Knickmeyer says. “When children see a mask, they don’t see it as social. It goes into that quick-and-dirty assessment part of the brain.”
As part of the study, the team also imaged the children’s brains using MRI technology. They found that the content of the microbial community at 1 year was associated with the size of the amygdala, which is part of the brain involved in making quick decisions about potential threats.
Connecting the dots suggests that the microbiome may influence how the amygdala develops and operates. That’s one of many interesting possibilities uncovered by this new study, which the team is currently working to replicate. Knickmeyer is also preparing to start up new lines of inquiry with new collaborations at IQ, asking new questions that she’s excited to answer.
“We have a great opportunity to support neurological health early on,” she says. “Our long-term goal is that we’ll learn what we can do to foster healthy growth and development.”
Source: Michigan State University