Pro-healing macrophages may help to regrow damaged nerves, a new study with rats suggests.
The approach, researchers say, comes close to equaling the current best treatment—a surgical transplant using a nerve stripped from another part of the patient’s body.
Macrophages are known as the “Pac-Man” of the immune system and form the body’s first line of defense against invasion—they indiscriminately engulf and eat most anything deemed a dangerous trespasser, whether it’s a bacterium or cellular debris from deceased tissue. Recent research, however, has shown that some macrophages also promote healing.
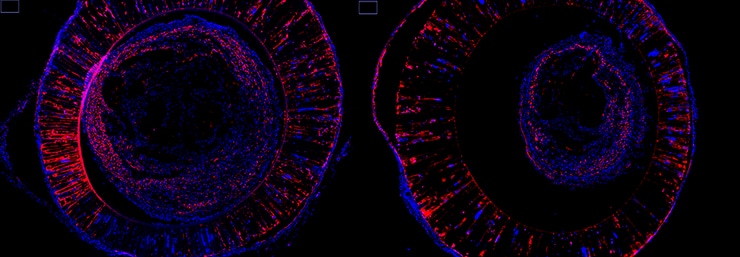
In a study in the Proceedings of the National Academy of Sciences, researchers have shown that summoning these pro-healing macrophages can greatly help regrow severed nerves in rats.
“There’s been a long-held view that the best way to regrow severed nerves is to provide all sorts of matrix and growth proteins to coax repair,” says Ravi Bellamkonda, professor of biomedical engineering and Vinik Dean of the Pratt School of Engineering at Duke University.
“We’ve completely shifted that view by finding new players who have remained behind the scenes. We believe this approach will also have a major impact on regenerative medicine, even beyond this specific application.”
The peripheral nervous system includes nerves that run from the spinal cord to the rest of the body. It connects and controls movements, the digestive system, heart, lungs, and other organs. When these relatively long cells—which can stretch for a meter or more—are damaged or severed, the injury is not easily healed.
The current standard of care, called an autograft, involves surgically removing a less important nerve, like the one running down the back of the calf, and grafting it into the damaged area. But the treatment has several drawbacks.
A sensory neuron replacing a motor neuron is not a perfect replacement, painful neuromas can occur at the healing site, the patient loses the function of another nerve, and, in the case of extensive injuries, there are only so many semi-disposable nerves in the body to harvest.
Researchers have long been working on an alternative approach using “nerve bridges” to span these gaps. The idea is to introduce a tube filled with growth factors and other goodies across the gap to coax the regrowth of the existing nerve, like luring a dog out of a hiding place with treats. But despite efforts to find the optimal combination of tube material, growth factors, proteins, and other helpers, nothing has come close to matching the autograft’s success.
Bellamkonda and his group were traveling down this same road until some salamanders lost their tails.
“We saw a study showing that the early presence of macrophages were vital to a salamander’s ability to regenerate its tail,” says Nassir Mokarram, an assistant research professor of biomedical engineering. “We also knew that rare instances of nerve regeneration were accompanied by a surge of these cells right after the injury occurred. Those two observations gave us the inspiration to see if the same idea could be applied with nerve bridges.”
Can saving axons keep nerves alive?
In 2012, Bellamkonda and Mokarram showed that nerve regeneration could be increased in rats by forcing macrophages to become the pro-healing variety that secrete healing compounds. In the new paper, the researchers take their work a step further.
Instead of issuing orders to make mature macrophages switch roles, they filled the nerve bridge with a biological signal shown to attract younger, undifferentiated cells destined to become pro-healing macrophages.
“Instead of retraining the demolition and cleanup crew, we hired a new workforce with a future in construction,” says Mokarram.
“The results were significantly better. This is the closest anyone has ever been to equaling the efficacy of an autograft, and we did it with nothing more than a tube and the recruitment of the body’s own immune system,” he says.
The researchers next plan to test the approach using a specialized nanofiber material they developed that has already proven better at bridging nerve endings than the tubes used in this proof-of-concept study.
Drug for MS could also treat nerve damage
“We’re the first group to prove this immunological approach to healing works with nerves in rodents,” says Mokarram. “We think this work will open a path to using similar methods in the much more complex and difficult arenas of the spinal cord and brain.”
The National Institutes of Health supported this work, which was done in close collaboration with a biologist at Emory University.
Source: Duke University



