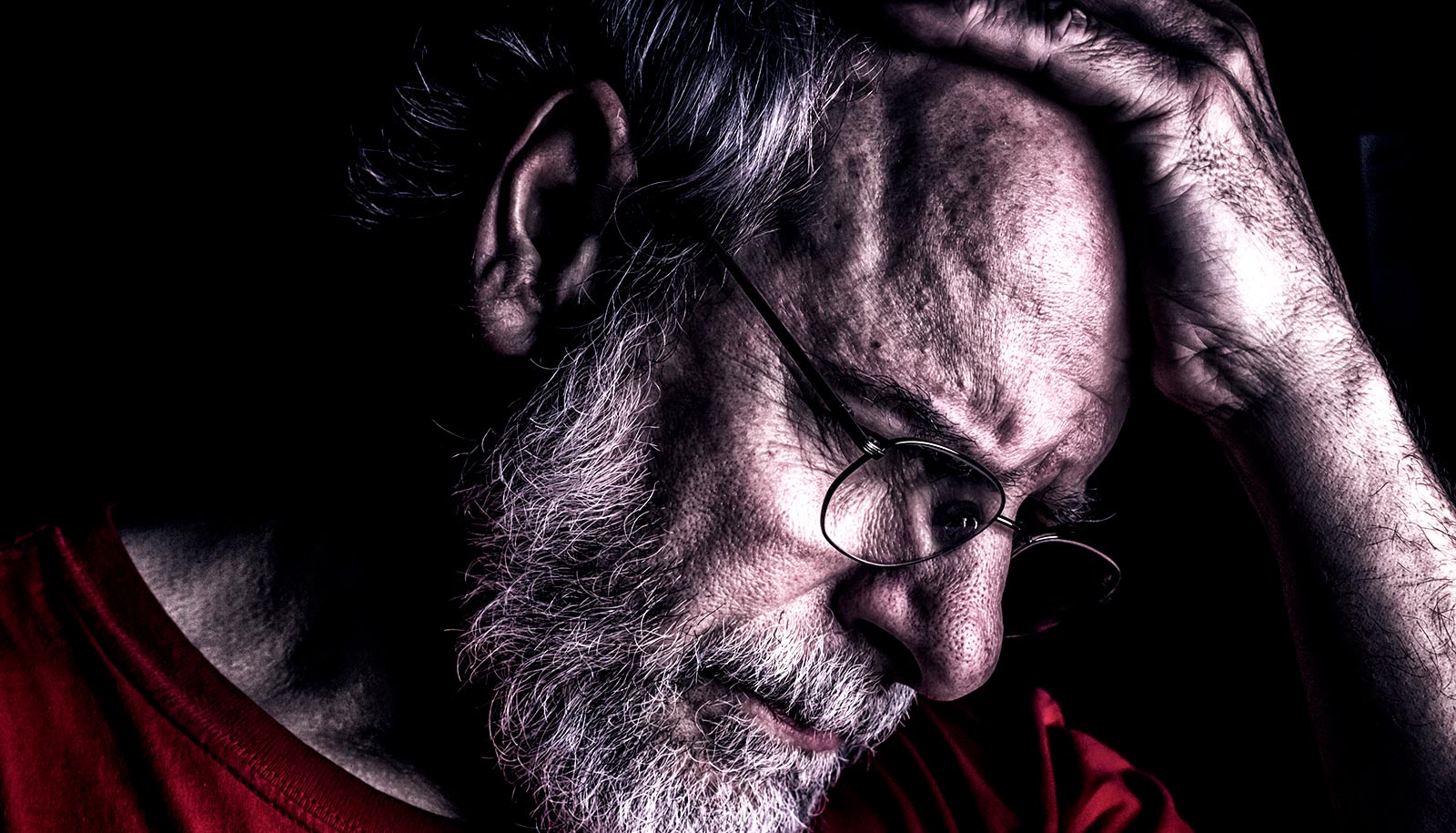
Sensory neurons that serve the head and face are wired directly into one of the brain’s principal emotional signaling hubs, research finds.
This accounts for why people consistently rate pain of the head, face, eyeballs, ears, and teeth as more disruptive, and more emotionally draining, than pain elsewhere in the body.
“Usually doctors focus on treating the sensation of pain, but this shows the we really need to treat the emotional aspects of pain as well.”
Sensory neurons elsewhere in the body are also connected to this hub, but only indirectly.
The results may pave the way toward more effective treatments for pain mediated by the craniofacial nerve, such as chronic headaches and neuropathic face pain.
“Usually doctors focus on treating the sensation of pain, but this shows the we really need to treat the emotional aspects of pain as well,” says Fan Wang, a professor of neurobiology and cell biology at Duke University, and senior author of the study.
Two different groups of sensory neurons carry pain signals from the head and from the body to the brain, and it is possible that neurons from the head are simply more sensitive to pain than neurons from the body.
But differences in sensitivity would not explain the greater fear and emotional suffering that patients experience in response to head-face pain than body pain, Wang says.
Functional Magnetic Resonance Imaging (fMRI), which shows greater activity in the amygdala—a region of the brain involved in emotional experiences—backs up personal accounts of greater fear and suffering in response to head pain than in response to body pain.
“There has been this observation in human studies that pain in the head and face seems to activate the emotional system more extensively,” Wang says. “But the underlying mechanisms remained unclear.”
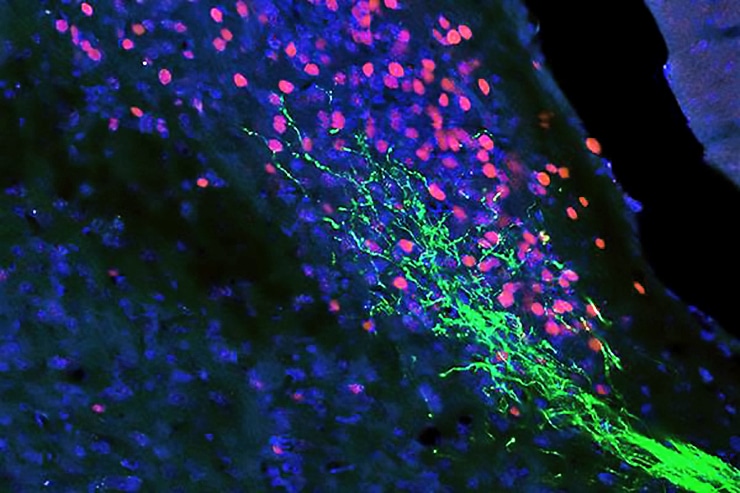
To examine the neural circuitry underlying the two types of pain, Wang and her team tracked brain activity in mice after irritating either a paw or the face. They found that irritating the face led to higher activity in the brain’s parabrachial nucleus (PBL), a region that is directly wired into the brain’s instinctive and emotional centers.
Then they used methods based on a novel technology Wang’s group recently pioneered, called CANE, to pinpoint the sources of neurons that caused this elevated PBL activity.
“It was a eureka moment because the body neurons only have this indirect pathway to the PBL, whereas the head and face neurons, in addition to this indirect pathway, also have a direct input,” Wang says. “This could explain why you have stronger activation in the amygdala and the brain’s emotional centers from head and face pain.”
Placebo ‘sweet spot’ could help control your pain
Further experiments showed that activating this pathway prompted face pain, while silencing the pathway reduced it.
“We have the first biological explanation for why this type of pain can be so much more emotionally taxing than others,” says Wolfgang Liedtke, a professor of neurology at Duke University Medical Center and a coauthor on Wang’s paper, who is also treating patients with head- and face-pain.
“This will open the door toward not only a more profound understanding of chronic head and face pain, but also toward translating this insight into treatments that will benefit people,” say Liedtke.
Chronic head-face pain such as cluster headaches and trigeminal neuralgia can become so severe that patients seek surgical solutions, including severing the known neural pathways that carry pain signals from the head and face to the hindbrain. But a substantial number of patients continue to suffer, even after these invasive measures.
“Some of the most debilitating forms of pain occur in the head regions, such as migraine,” says Qiufu Ma, a professor of neurobiology at Harvard Medical School, who was not involved in the study. “The discovery of this direct pain pathway might provide an explanation why facial pain is more severe and more unpleasant.”
Liedtke says targeting the neural pathway researchers identified here could be a new approach toward developing innovative treatments for this devastating head and face pain.
Can green LED light ease your chronic pain?
The researchers report their results in Nature Neuroscience.
Grants from the National Institutes of Health supported this research. Liedtke is also supported by the Facial Pain Research Foundation (Gainesville, Florida).
Source: Duke University