Using a simulation modeling approach, researchers estimate that closing syringe services programs, even for one year, will cause cases of HIV to rise.
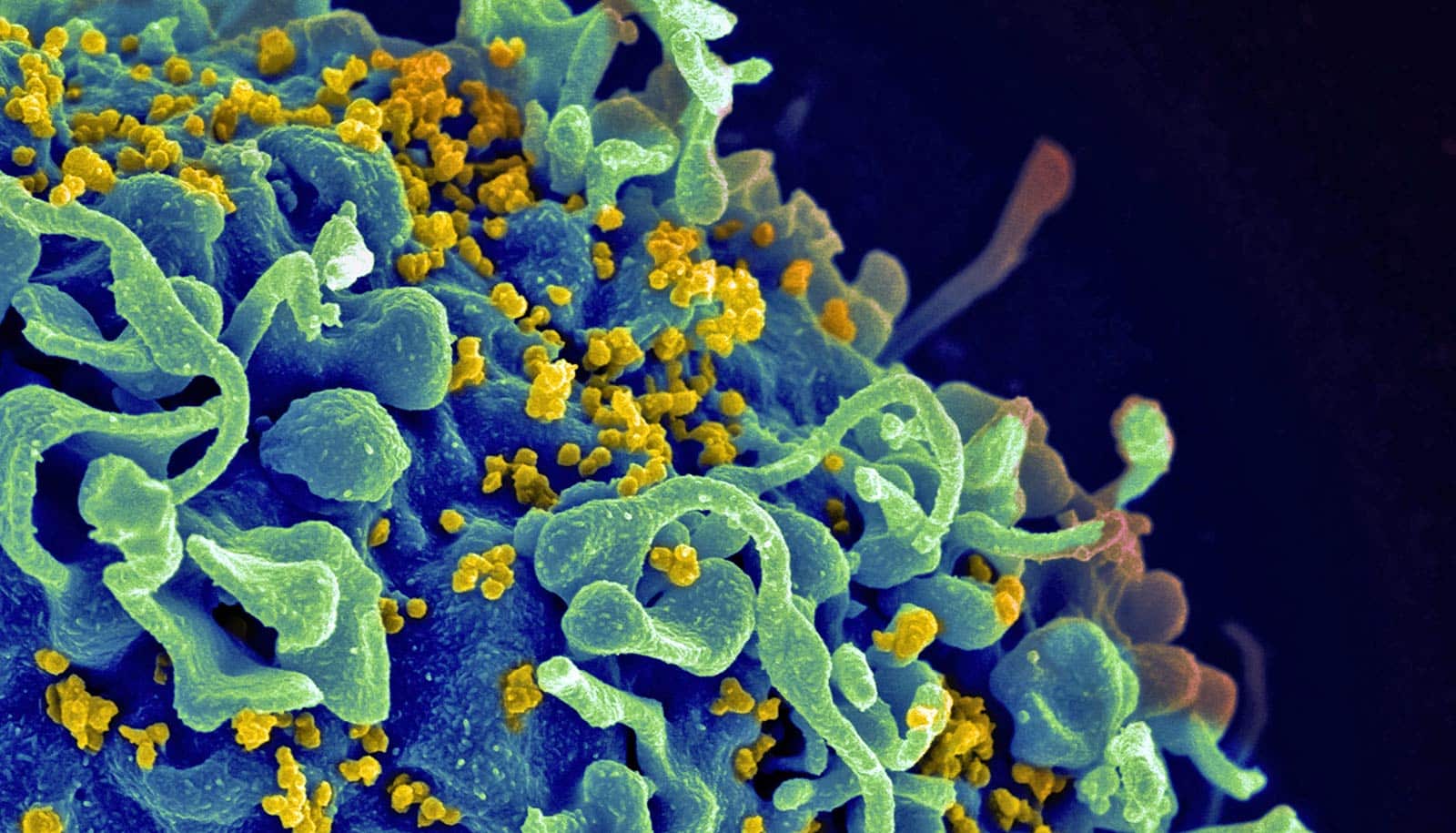
Syringe services programs—sites where people who use drugs can access sterile syringes and dispose of injection equipment—often face political backlash. But the new study shows the effectiveness of these programs in both curbing HIV transmission among people who use drugs and preventing future outbreaks.
In a rural American setting that had previously experienced one of the largest HIV outbreaks among people who use drugs, a simulation suggested that closing the existing syringe services programs would likely lead to a rebound HIV outbreak, with an almost 60% increase in infections among people who use drugs in five years.
Even closing the program temporarily would lead to an increase in cases of HIV, the study shows.
“Our work shows that shutting down syringe services programs has immediate and detrimental impacts on people who use drugs and the broader community,” says senior author Brandon Marshall, an associate professor of epidemiology at Brown University. “We should be expanding access and increasing sustainable funding to these programs to prevent future outbreaks.”
The analysis in the journal AIDS presents the first study to the researchers’ knowledge to quantitatively examine the impact of syringe services program closure on HIV incidence.
Syringe services programs are community-based prevention programs that provide services such as referrals to substance use disorder treatment, access to and disposal of sterile syringes and injection equipment, and vaccination, testing, and connections to care for infectious diseases. They’re effective in curbing the transmission of HIV—as long as they remain in operation, the researchers say.
In 2015, Scott County, Indiana, experienced one of the largest outbreaks in the US of HIV among people who use drugs: Out of fewer than 24,000 residents, 181 people were diagnosed with HIV infection, corresponding to an incidence rate over 50 times the national average.
In response, the county implemented a syringe services program that had to be renewed every two years. As the two-year deadline approached and the Scott County commissioners voted to end the program, the researchers set up a simulation modeling study to estimate the impact of the program closure.
The researchers created a model to simulate HIV risk behaviors and transmission in adults in Scott County who inject drugs as well as those who do not. They projected HIV incidence and prevalence between 2020 and 2025 for four scenarios: persistent program operation (no pause; no closure); permanent closure; delayed closure (after two years); and temporary closure (for 12 months).
According to lead study author Xiao Zang, a postdoctoral research associate in epidemiology, the idea underlying the model was to replicate the epidemic in Scott County, including the number of people participating in the syringe services program and the benefits they received.
The researchers worked with the Scott County Department of Health to obtain local data for the program, and also used behavioral data to find estimates of how often people who inject drugs share injections. To make sure the model was accurately replicating reality, Zang says that the team made substantial efforts to calibrate their model against local surveillance data from the Indiana State Department of Health, which reports the number of new HIV diagnoses each year as well as mortality among people with HIV.
The analysis found that compared to sustained operation, permanently closing the syringe services program would result in an average increase of 63.5 HIV infections over a five-year period, an increase of 58.4%. Among people who inject drugs, suspending the program permanently would result in an average of 60.2 more infections (an increase of 161%), growing the existing high level of prevalence (48% in 2019 based on model estimates) to even higher at 60.8%.
If the program closure was delayed by two years, the researchers estimated 42.4 additional HIV infections (a 38.9% increase) compared with sustaining operation. In the model of temporary closure for one year (April 2020 to March 2021), they estimated an average of 11.6 (35.3%) more infections during 2020-2021.
“Our analysis shows that even a short-term service disruption may cause a spike in HIV incidence,” Zang says.
The implications of the research can be generalized to other rural counties across the US, Zang says, especially those identified by the US Centers for Disease Control and Prevention as vulnerable to rapid HIV transmission. Zang adds that this type of simulation can help communities make health policy decisions in the absence of timely data.
“This simulation model provides another way of examining and evaluating health policy impact of interventions in the real world,” Zang says. “We hope that these results will help decision-makers understand the devastating impact that closing a center will have on the community.”
Additional researchers from Brown, in collaboration with scientists from Boston University, Yale University, New York University, and Simon Fraser University in Canada.
Funding for this study came from the National Institutes of Health.
Source: Brown University