A new gene therapy turns glial cells—abundant support cells in the brain—into neurons, repairing damage that results from stroke and significantly improving motor function in mice.
Once researchers further develop the NeuroD1-based gene therapy, it could potentially help to treat stroke, which is a leading cause of disability in the US, with 800,000 new stroke patients every year.
“The current treatment for stroke has a narrow time window, typically within a few hours after the occurrence of stroke,” says lead author Yuchen Chen, a postdoctoral fellow at Penn State. “Many patients cannot receive the treatment in time and as a result, often suffer from permanent disability caused by irreversible neuronal loss. There is an urgent need to develop a new therapy to regenerate new neurons and restore lost brain functions among stroke patients.”
The human brain has approximately 86 billion neurons. While mini-strokes can be tolerated, moderate stroke involving the loss of billions of neurons leaves detrimental effects that do not spontaneously recover.
“So, the critical question that is still unanswered in the neuroregeneration field is how can we regenerate billions of new neurons in a patient’s brain after stroke?” says Gong Chen, professor of biology and chair in life sciences. “The biggest obstacle for brain repair is that neurons cannot regenerate themselves. Many clinical trials for stroke have failed over the past several decades, largely because none of them can regenerate enough new neurons to replenish the lost neurons.”
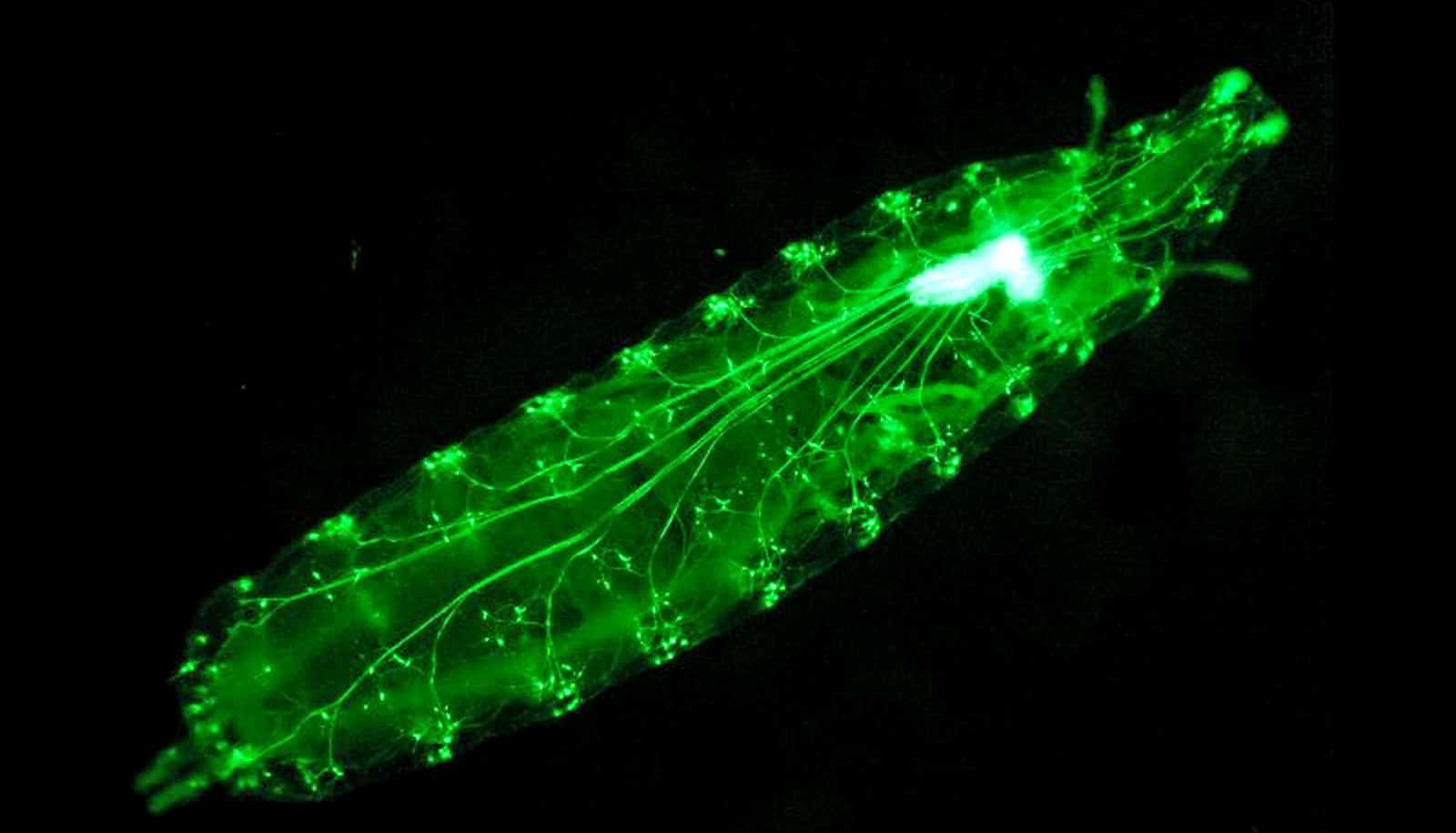
The reserchers pioneered a new approach to regenerate functional neurons using glial cells, a group of cells surrounding every single neuron in the brain that provide essential support to neurons. Unlike neurons, glial cells can divide and regenerate themselves, especially after brain injury.
“I believe that turning glial cells that are already present in the brain into new neurons is the best way to replenish the lost neurons,” says Gong Chen. “These glial cells are the neighbors of the dead neurons in the brain and are likely to share the same ancestral cellular lineage.”
The team previously reported that a single genetic neural factor, NeuroD1, could directly convert glial cells into functional neurons inside mouse brains with Alzheimer’s disease, but the total number of neurons generated was limited. The research team believed that this limited regeneration was due to the retroviral system used to deliver NeuroD1 to the brain.
In the current study, the research team used the AAV viral system, which is now the first choice for gene therapy in the nervous system, to deliver NeuroD1 into mouse motor cortex that a stroke had damaged.
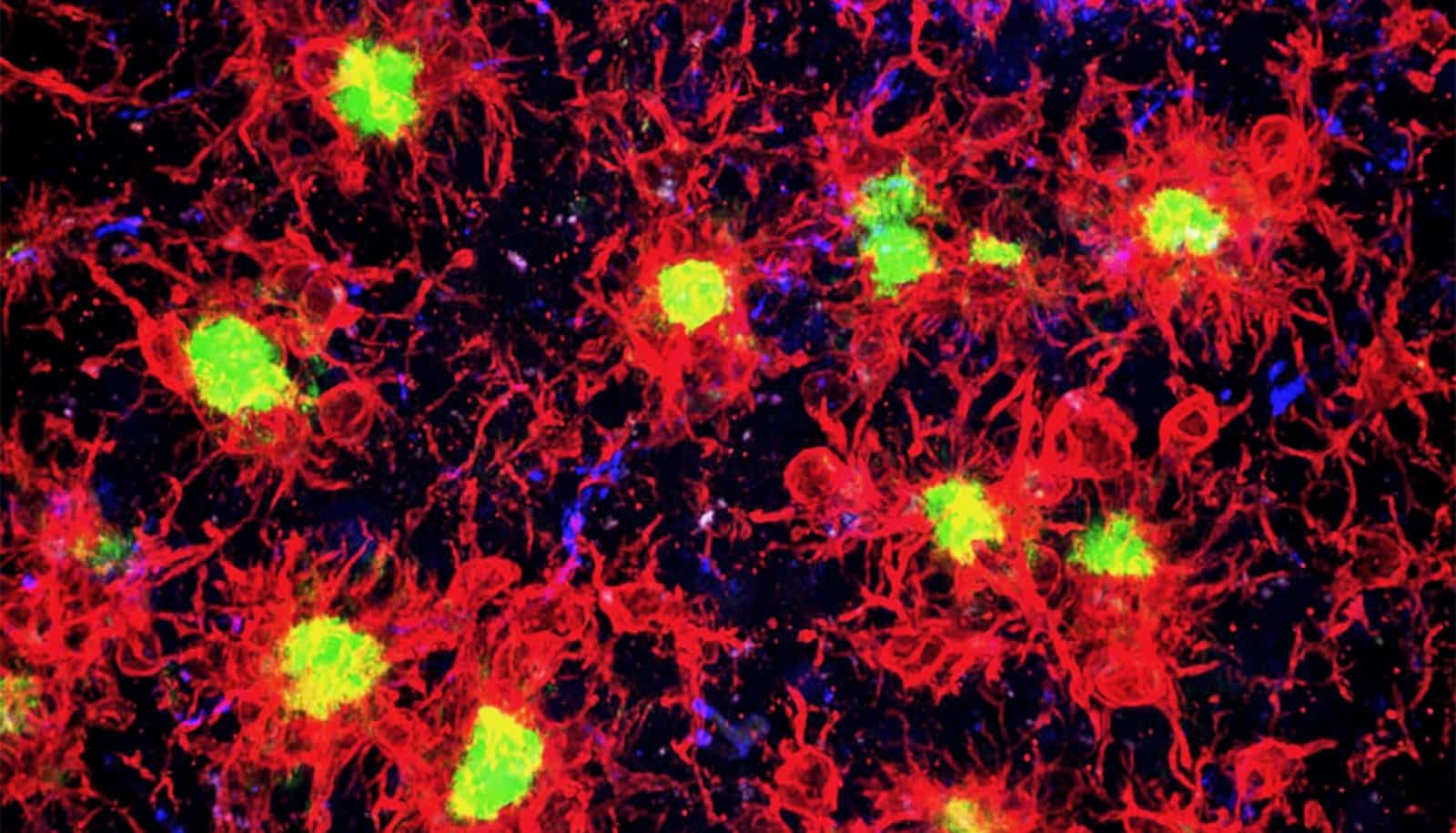
Many neurons die after stroke but surviving glial cells can proliferate and form a glial scar in the stroke areas. The researchers designed their AAV system to express NeuroD1 preferentially in the glial cells that form these scars, turning them directly into neuronal cells. Such direct glia-to-neuron conversion technology not only increased neuronal density in the stroke areas, but also significantly reduced brain tissue loss the stroke caused.
Interestingly, the newly converted neurons showed similar neuronal properties to the neurons that were lost after stroke. This suggests a potential impact of the local glial lineage on the converted neuronal identity.
“The most exciting finding of this study is to see the newly converted neurons being fully functional in firing repetitive action potentials and forming synaptic networks with other preexisting neurons,” says Gong Chen. “They also send out long-range axonal projections to the right targets and facilitate motor functional recovery.”
A separate collaborative work led by Gregory Quirk, a professor at the University of Puerto Rico, further tested the NeuroD1-based gene therapy in a rat stroke model. Quirk and colleagues also found that this direct glia-to-neuron conversion technology can rescue cognitive functional deficits stroke induces.
“Because glial cells are everywhere in the brain and can divide to regenerate themselves, our study provides the proof-of-concept that glial cells in the brain can be tapped as a fountain of youth to regenerate functional new neurons for brain repair not only for stroke but also for many other neurological disorders that result in neuronal loss,” says Yuchen Chen. “Our next step is to further test this technology and ultimately to translate it into clinically effective therapies to benefit millions of patients worldwide.”
A paper describing the new therapy appears in the journal Molecular Therapy.
Additional researchers at Penn State and the University of Puerto Rico contributed to the work. The US National Institutes of Health and the Penn State Charles H. Skip Smith Endowment Fund supported the research.
Source: Penn State