A new study reveals that small cell lung cancer likely begins in basal stem cells rather than in neuroendocrine cells, marking a major shift in the understanding of this aggressive disease that is often associated with smoking.
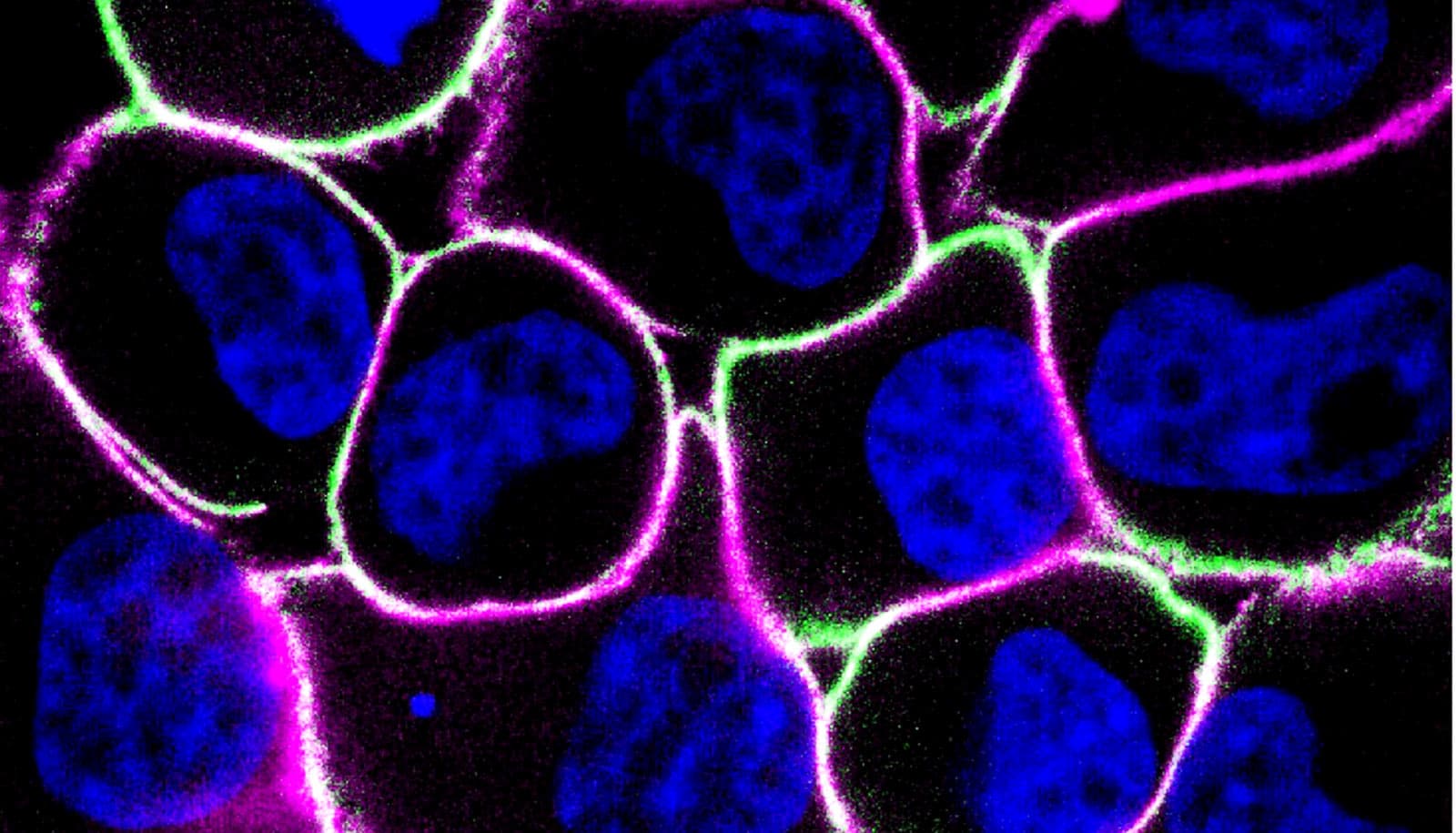
For decades, scientists have thought small cell lung cancer (SCLC) begins in specialized lung cells known as neuroendocrine cells. The study—led by Duke scientists and published in the journal Nature—shows basal cells (which have the ability to regenerate multiple lung cell types) can give rise to tumors in both the classic neuroendocrine form and a tuft-like form.
The tuft-like form is associated with poor patient outcomes and resistance to current therapies. By pinpointing that basal cells can form both tumor states, researchers can now explore strategies to prevent the disease before it evades the immune system and spreads.
“This discovery reshapes our understanding of how small cell lung cancer begins,” says the study’s senior author, Trudy G. Oliver, professor in the pharmacology and cancer biology department at Duke University School of Medicine.
“Our models, for the first time, reflect the full complexity of the disease,” Oliver says, “allowing us to study and target its most dangerous forms.”
Using genetically engineered mice, 3D tumor organoids, and the largest-available dataset of human SCLC tumors (at 944 samples), researchers also discovered the tuft-like tumors were only triggered when genetic changes were introduced into basal cells—not neuroendocrine cells—suggesting a fundamental shift in how scientists understand the disease.
“We used a technique called lineage barcoding that allowed us to tag individual cells and track how they evolve over time,” says the study’s first author, Abbie S. Ireland, graduate student in the Molecular Cancer Biology program at Duke University School of Medicine.
“This revealed that small cell lung cancer cells can shapeshift through a process called cell fate plasticity,” Ireland says, “which helps explain why the disease resists treatment and could provide new approaches for how we might block their transition into aggressive cancer.”
The researchers say this discovery creates the first accurate lab models of the most treatment-resistant tuft-like form of SCLC. The models, in combination with new foundational understanding, allow for advancement in the study of early detection and targeted therapies.
“We now have the tools to explore how the immune system interacts with these basal cells before they transform into aggressive cancer. That opens the door to therapies that could stop the disease before it even starts,” says Oliver.
Funding for the research came from the Duke Science and Technology Scholar initiative, the National Institutes of Health through National Cancer Institute grants, and the Cancer Center Support Grant.
Source: Duke University