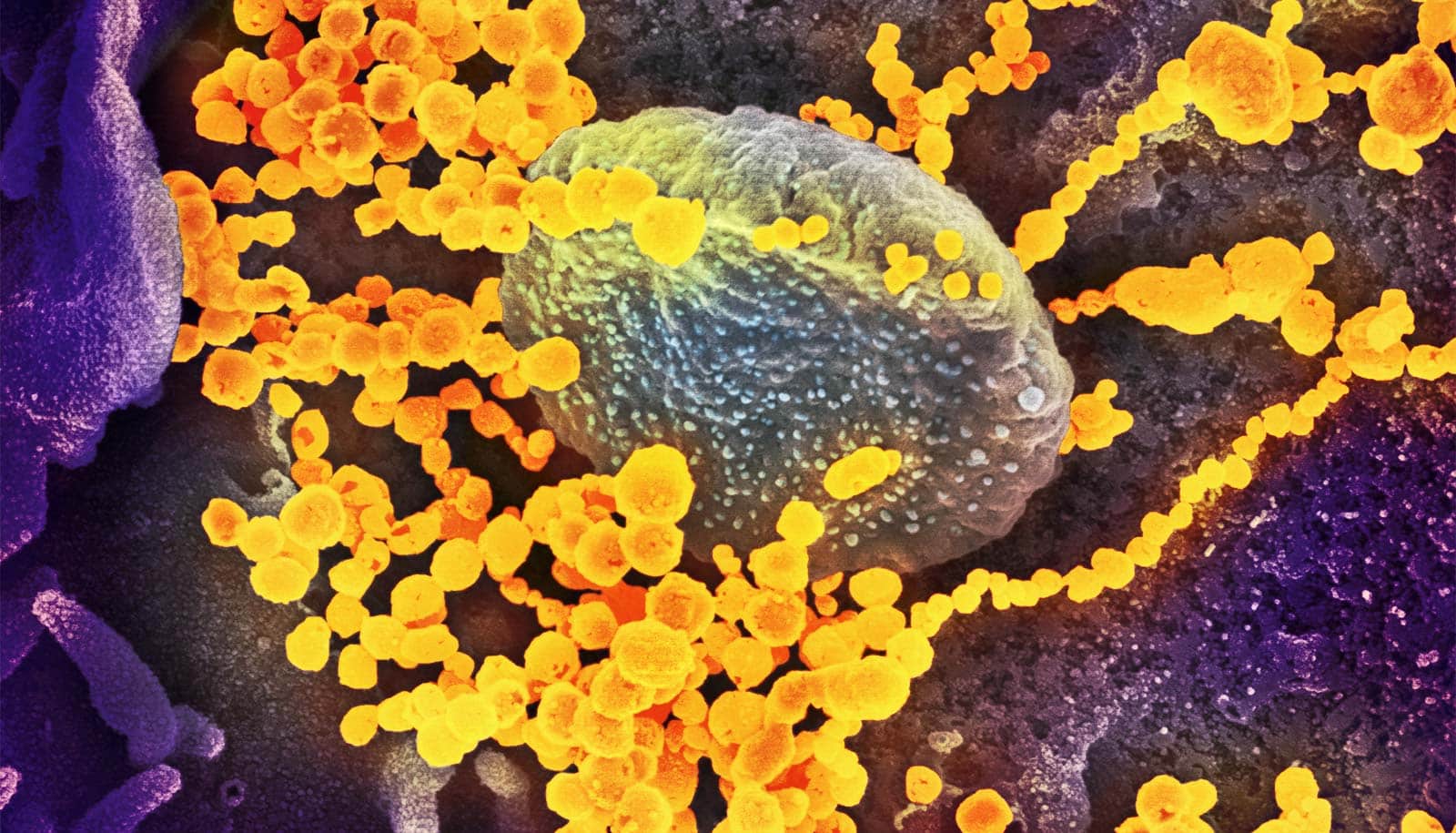
New research may reveal why women get severe COVID-19 at about half the rate as men.
Women have more of a certain type of immune cell that fights infections in mucosal tissue, and these immune cells amass in the lungs, poised to attack the COVID virus, according to a new study.
“Better armed with these specialized immune cells, women appear to be more equipped to fight some of the most severe impacts of COVID-19, notably the respiratory infections that can become life-threatening,” says Daniel Saban, an associate professor in the ophthalmology department and in the immunology department at Duke University.
Saban says the investigation began last spring as COVID first spread and he was sidelined from his normal caseload studying eye diseases. A piece of equipment in his lab—a device that can perform 36-color flow cytometry—was sitting idle, so he decided to use it to examine blood samples from COVID patients.
“We didn’t start with a hypothesis,” Saban says. “It was a completely unbiased approach, where we asked our colleagues to provide blood and tissue samples from COVID patients as well as healthy people. We had no idea what we would find, if anything.”
The researchers quickly saw that a white blood cell called mucosal associated invariant T cells, or MAIT cell, circulated more abundantly in the blood from healthy women compared to healthy men. MAIT cells are highly specialized white blood cells that contribute to immune defenses in mucosal organs and tissues.
Among COVID patients, however, there were few MAIT cells circulating in the blood, even among women, where the population of MAIT cells radically fell off, leading the researchers to question where these cells had gone.
They found their answer in tissue samples from the lungs of COVID patients. Overall, there were an abundance of MAIT cells in the lung tissue of people with COVID, but upon closer inspection, they found night-and-day differences between the sexes.
“We first found this dichotomy in healthy blood,” Saban says. “Circulating MAIT cells in women expressed genes indicative of a robust profile poised for fighting an infection, but this was not the case in males. Then we looked in the tissue and were able to find evidence of this same pattern by sex.”
Saban says there are numerous examples of sexual differences in the immune responses to infections, noting those differences have been prevalent all along with COVID-19.
“Our findings uncover a female-specific protective profile carried out by these MAIT cells, and this could potentially help guide the development of treatments and therapies,” he says.
The study appears in the journal Med.
Support for the study came from the National Institute of Allergy and Infectious Diseases, which is part of the National Institute of Health, the US Defense Advanced Projects Agency, the Veterans Affairs Health System, and Virology Quality Assurance.
Source: Duke University