A new test predicts sepsis soon after infection—well before blood clotting and organ failure—enabling early antibiotic treatment and markedly increased survival, a study with mice shows.
The findings provide a platform to develop rapid and easy-to-perform clinical tests for early sepsis detection and clinical intervention in human patients.
The researchers succeeded in detecting a catastrophic shift in blood protein abundance soon after infection that can predict sepsis well before disease symptoms and organ damage arise.
“Early detection is critical for clinical intervention to increase survival in sepsis patients.”
Sepsis is the number one cause of death in US hospitals. In the clinic, sepsis is diagnosed by a symptom-based approach that may include kidney or liver failure, blood clotting or bleeding—which often occurs well after permanent organ damage. Thus, molecular diagnostics that detect infection at early stages of disease to minimize host injury are sorely needed.
“The key finding was identifying proteins in the blood that arise very soon after infection—well before overt disease symptoms,” explains Michael Mahan, professor at the University of California, Santa Barbara. “Early detection is critical for clinical intervention to increase survival in sepsis patients.”
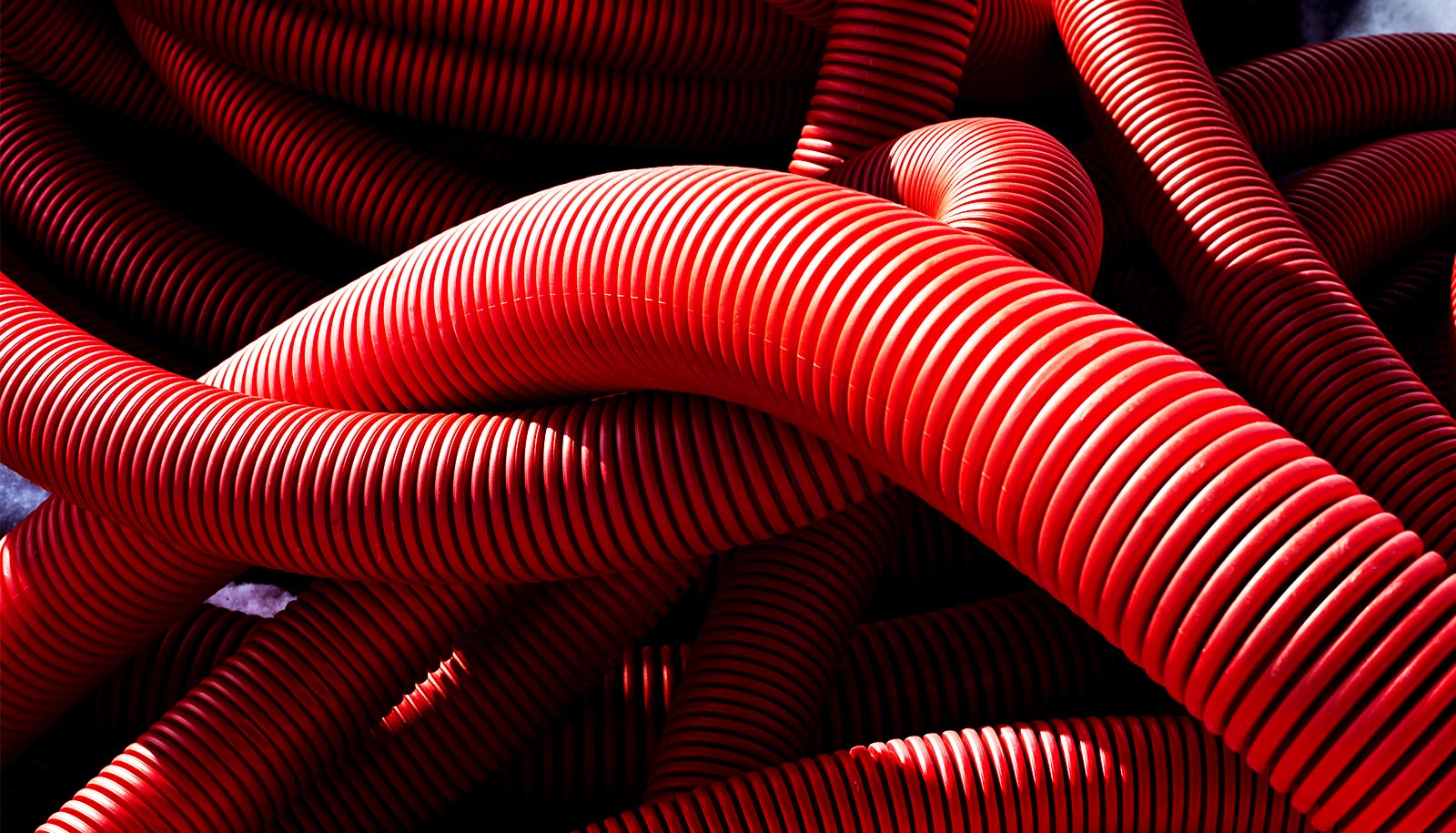
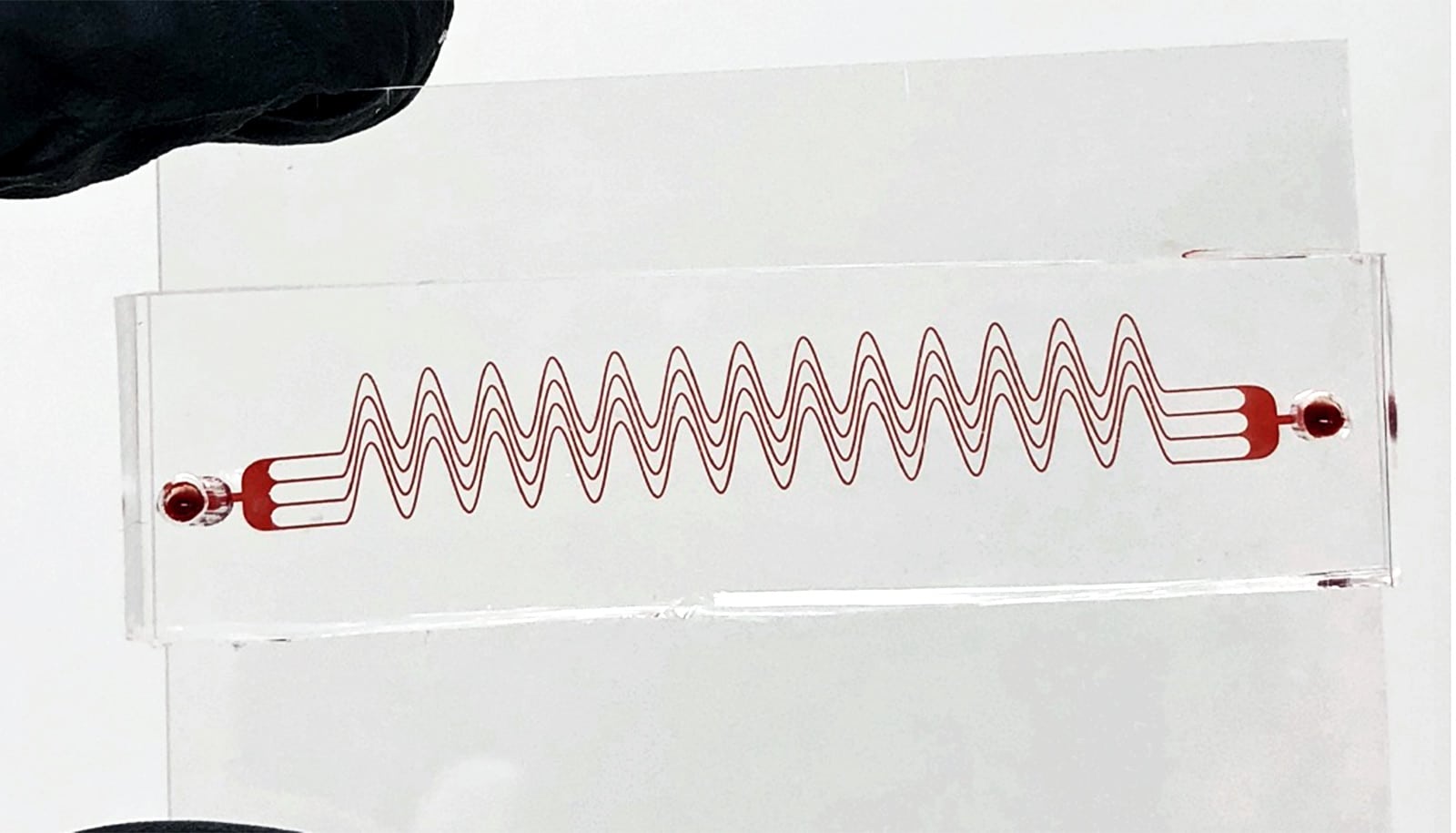
To carry out the test, researchers collected a small amount of blood and analyzed it for an increase in coagulation proteins that are induced but inactive at early stages of infection. Such detection enabled early antibiotic treatment—well before activated coagulation proteins induced blood clotting—resulting in markedly increased survival in mice. The technology is open source and freely accessible to all.
The study also shows that antibiotics are less effective after blood proteins increase in response to infection. Treatment failure may be due to host injury triggered by excessive blood clotting, providing insight into why delays in antibiotic treatment in human sepsis are associated with increased risk for death.
“The future plan is to identify a biopanel of early sepsis blood proteins for incorporation into existing blood tests, enabling sepsis prediction well before excessive blood clotting and permanent organ damage,” says coauthor Douglas Heithoff.
The researchers demonstrated that the changes in blood proteins soon after infection observed in mice were similar to that reported for human sepsis. Thus, they are optimistic that these findings are translatable for the early detection and treatment of sepsis in humans.
“Currently, one in four patients die of sepsis, with many survivors experiencing lifelong debilitation with cognitive decline,” coauthor Scott Mahan says. “We hope technologies like this offer new ways of delivering state-of-the-art molecular diagnostics that predict sepsis before permanent injury occurs.”
The paper appears in eBioMedicine. Additional coauthors are from UC San Diego, Sanford Burnham Prebys Medical Discovery Institute (SBPMDI), and UC Santa Barbara.
The National Institutes of Health’s National Heart, Lung, and Blood Institute; Santa Barbara Cottage Hospital; and the US Army Research Office funded the work.
Source: UC Santa Barbara