Good airflow and filtration in schools may help children with intellectual and developmental disabilities and their teachers avoid COVID infections, a new study finds.
During the pandemic, researchers from the University of Rochester Medical Center (URMC), the Intellectual and Developmental Disabilities Research Center (IDDRC), and the Mary Cariola Center, a special education school in Rochester, NY, looked at ways to study ways to prevent COVID infection among these children, a particularly vulnerable population.
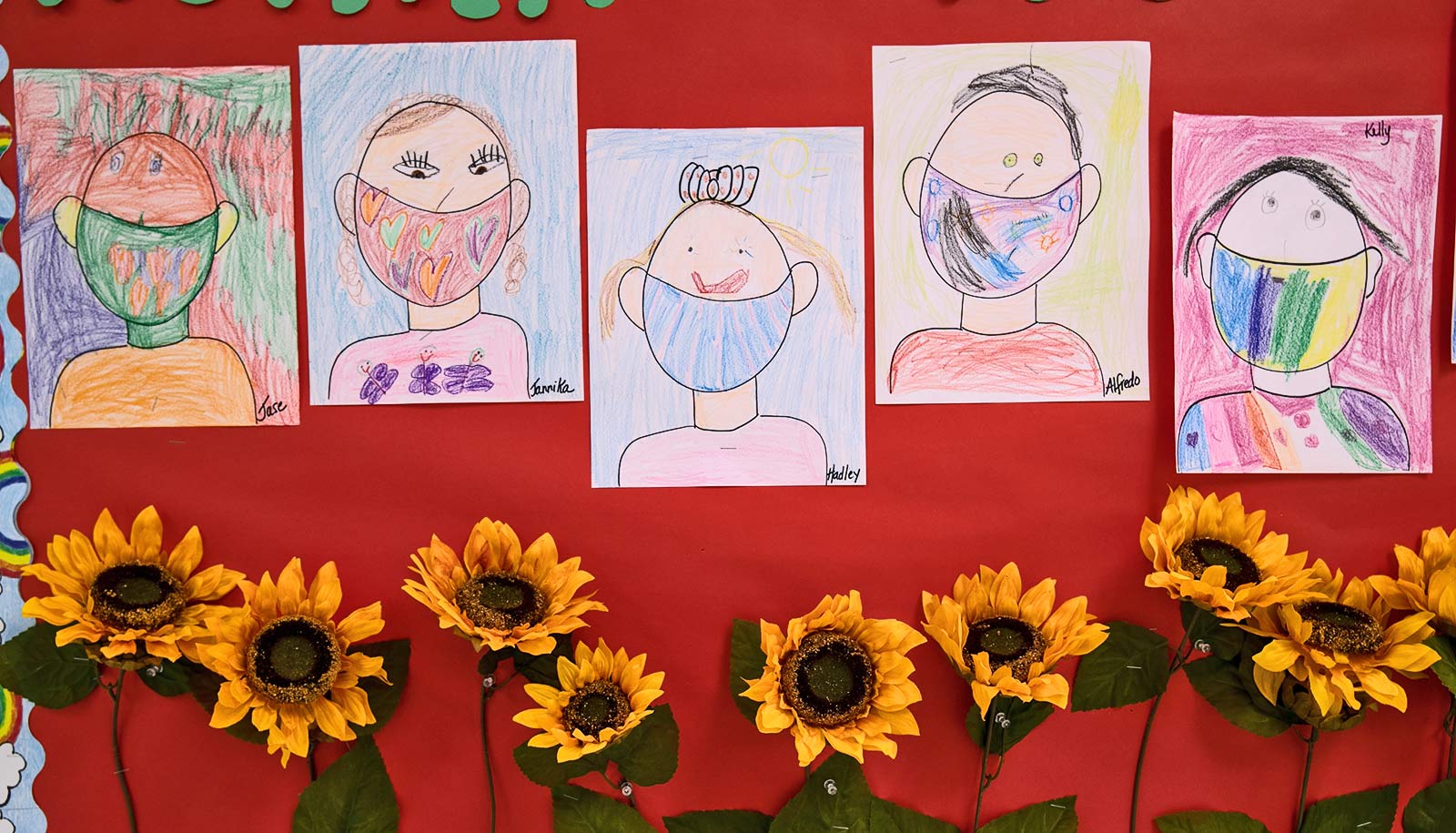
The COVID pandemic was a particularly difficult balancing act for children with intellectual and developmental disabilities (IDDs) and their families. The Mary Cariola Center serves more than 450 students ages 3-21 with severe IDDs and complex medical needs. Many of these children are at heightened risk for infection, but they may also struggle with protective measures, like masking and distancing.
Many students rely on the Center for needed services and therapy, so it was imperative to keep these kids in school—and to make sure school was as safe as possible.
To expand the limited COVID prevention toolbox available to these children, URMC researchers and Mary Cariola Center administrators turned their attention toward airflow and filtration in the school.
“COVID, like flu and RSV, is primarily spread through the air,” says Martin Zand, professor of medicine and senior associate dean for clinical research at URMC, who co-led the study. “The virus that causes COVID can circulate in the air for up to three hours, so the quicker you filter or circulate out that air, the better.”
Zand and colleagues measured levels of carbon dioxide, a gas we breathe out, in 100 rooms across three buildings on the Mary Cariola Center campus. While not a direct measure, carbon dioxide offers a relatively easy way to estimate ventilation: lower levels of carbon dioxide indicate better ventilation and air quality.
All 100 rooms, which varied in size and purpose—including small classrooms, therapy rooms, offices, and large activity rooms and gyms—stayed well below the Occupational Safety and Health Administration’s carbon dioxide limit. Only three rooms appeared to have lower ventilation (carbon dioxide levels over 2,000 parts per million) for two or more hours during the testing period, which lasted one to three days.
However, many rooms reached moderate carbon dioxide levels (1,001-2,000 parts per million), which are generally safe but may indicate less-than-optimal airflow.
According to the study, the number of COVID cases recorded among people who spent time in a given room was linked to the amount of time that room had moderate carbon dioxide levels (i.e. suboptimal ventilation).
The researchers also found a link between COVID cases and air filtration. One building on the Mary Cariola campus has a relatively new ventilation system that can support high-efficiency air filters, called MERV-13, which can capture more virus particles. The other two buildings have older systems that aren’t strong enough to move air through the tighter, high-efficiency filters. These systems use more porous MERV-11 filters that may allow more virus particles to circulate through the buildings.
The researchers found classrooms that relied on the more porous air filters had higher numbers of total COVID cases. However, the study was not designed to test if infections were acquired in or outside of school.
Since conducting the study, the Mary Cariola Center has been working on several fronts to improve ventilation in any areas of concern across their campus. They have also pursued state funding and begun conversations with property owners to make overall improvements to the ventilation systems.
While this study, published in PLOS ONE, focused on testing airflow and filtration, it was part of a larger project funded by the National Institutes of Health Rapid Acceleration of Diagnostics-Underserved Populations program.
That project, collaboratively led by Zand, John Foxe, director of the Del Monte Institute for Neuroscience and co-director of the UR-IDDRC, and Stephen Dewhurst, vice dean for research at the University of Rochester, brought COVID testing to students and staff in the Mary Cariola Center and helped catch cases early to prevent spreading.
“One thing that COVID taught us is that there isn’t one single magic solution that will prevent all infection from all viruses,” says Zand. “Rather, a combination of approaches is most effective, including masking, vaccination, ventilation, and air filtration.”
Source: University of Rochester