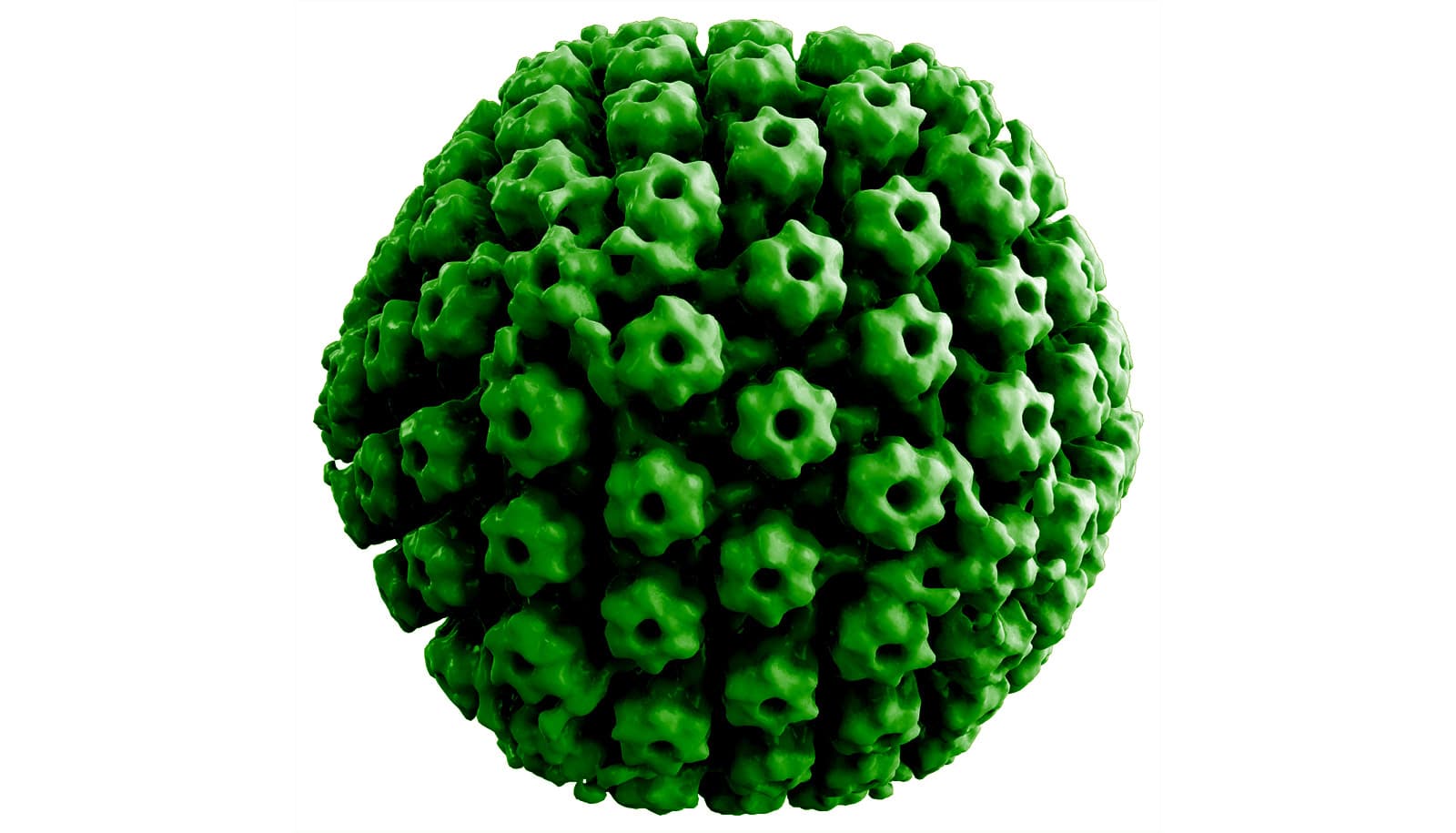
People with schizophrenia can have higher levels of antibodies against Epstein-Barr virus, a herpes virus that causes infectious mononucleosis, new research suggests.
Researchers didn’t design the study to pinpoint cause and effect, but say there are at least two possible explanations: Schizophrenia might alter immune systems and make patients more susceptible to the Epstein-Barr virus, or EBV infection might increase the risk of schizophrenia.
“We are interested in the role of infectious agents such as Epstein-Barr virus in schizophrenia and other serious psychiatric disorders, so we did this study to look at the associations,” says Robert Yolken, professor of neurovirology at the Johns Hopkins Children’s Center and senior author of the study, which appears in Schizophrenia Bulletin.
People with schizophrenia display distorted thinking, perception, emotions, language, sense of self, and behavior. Schizophrenia affects more than 21 million people worldwide, according to the World Health Organization.
Genetic risk
Epstein-Barr virus is the most common cause of infectious mononucleosis. The Centers for Disease Control and Prevention report that at least one of four teenagers and young adults infected with EBV will develop mono; its symptoms include extreme fatigue, fever, sore throat, and head and body aches. The virus is commonly transmitted through oral contact, such as kissing.
While schizophrenia has some genetic associations, genes researchers have identified so far explain only a portion of the disease risk. Previous studies have also identified environmental exposures, including some infectious agents, that increase the risk for schizophrenia.
The researchers studied 743 people, 432 with a schizophrenia diagnosis and 311 controls without a history of a psychiatric disorder.
The researchers compared EBV antibody levels in healthy people with those of people who have schizophrenia. People with schizophrenia were 1.7 to 2.3 times more likely to have increased levels of some EBV antibodies than people without the disease. Schizophrenia patients did not, however, have elevated levels of antibodies to related viruses, such as varicella/chicken pox or herpes simplex type 1/cold sore virus.
Further, people who had both evidence of increased genetic risk for schizophrenia and increased antibody levels to EBV had a more than eight times higher chance of being in the schizophrenia group.
Future treatments?
“We found that individuals with schizophrenia had an unusual response to Epstein-Barr virus,” Yolken says. “This indicated that the prevention and treatment of Epstein-Barr virus might represent an approach for the prevention and treatment of serious psychiatric disorders such as schizophrenia.”
The Food and Drug Administration has not approved any treatments for EBV, but researchers are investigating compounds that may prevent or treat replication of the virus. In the meantime, researchers say that good hygienic practices such as hand-washing and avoiding oral contact, such as kissing, with infected people could help prevent EBV transmission.
Additional researchers are from Johns Hopkins, Sheppard Pratt Health System, VanPelt Biosciences, and the Broad Institute of MIT and Harvard. The National Institute of Mental Health and Stanley Medical Research Institute funded the work.
Source: Johns Hopkins University