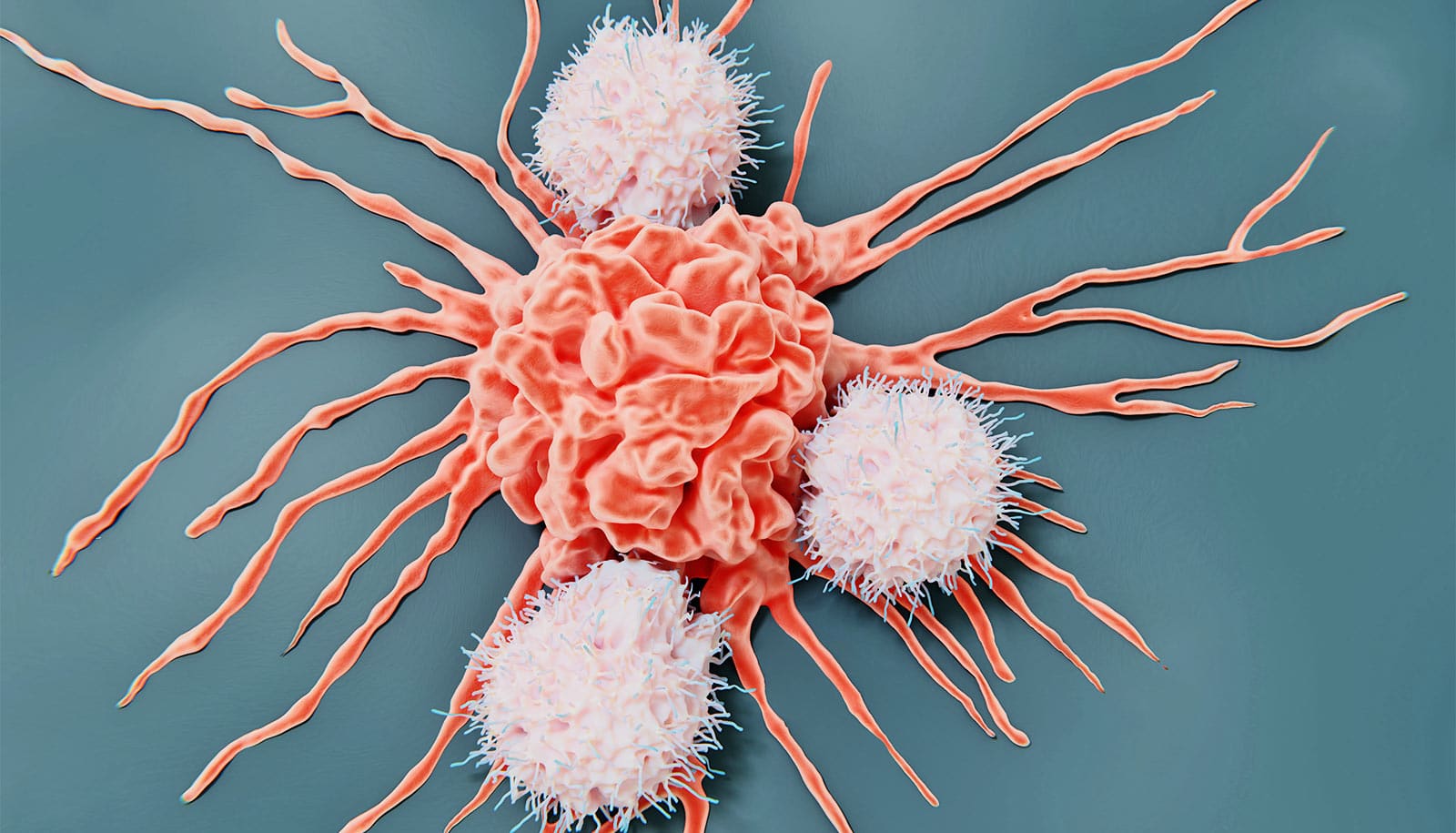
A new discovery confirms that a key molecule can reprogram immune cells that normally protect against infection and cancer, turning them into bad guys that promote cancer growth.
Studying the behavior of these “pro-tumor” immune cells is important because they could be targets for therapies that block their harmful activity, says Minsoo Kim, corresponding author of the study and a research leader at the University of Rochester’s Wilmot Cancer Institute.
Kim led a team of scientists investigating the dynamic interactions that occur between cells in the tumor environment, and the underlying factors that cause the harmful transformation of immune cells from good to bad.
They found that PAF (platelet-activating factor) is the key molecule that controls the destiny of the immune cells. PAF not only recruits cancer-promoting cells, but it also suppresses the immune system’s ability to fight back. In addition, they found that multiple cancers rely on the same PAF signals.
“This is what could be most significant,” says Kim, a professor of microbiology and immunology at the University of Rochester Medical Center. “Because if we find a treatment that could interfere with PAF, it could potentially apply to many types of cancer.”
Much of the team’s work focused on pancreatic cancer cells. It is one of the most deadly cancers, with a five-year survival rate of about 12%, and is notoriously hard to treat because pancreatic tumors are surrounded by a toxic stew of proteins and other tissues that protect the cancer from the immune system’s natural role to attack invaders. They also studied breast, ovarian, colorectal, and lung cancer cells, using advanced 3D imaging technology to watch the behavior of immune cells as they swarmed to the cancerous region.
Ankit Dahal, a member of Kim’s lab and a student in the UR Medical Scientist Training Program, designed the research project and wrote the journal article with Kim.
The research appears in the Proceedings of the National Academy of Sciences (PNAS).
The National Institutes of Health funded the study.
Source: University of Rochester