New research that clarifies how bacteria-infecting viruses disarm pathogens could lead to new treatment methods for bacterial infections.
Bacterial infections pose significant challenges to agriculture and medicine, especially as cases of antibiotic-resistant bacteria continue to rise.
In the new study in Science, Lanying Zeng, a professor, and Junjie Zhang, an associate professor, both from the Texas A&M College of Agriculture and Life Sciences biochemistry and biophysics department, and colleagues, detail a precise mechanism by which phages disable bacteria.
Together, the team worked to explain a series of interactions scientists have sought to understand since the early 1970s.
Phage therapy instead of drugs?
Pseudomonas aeruginosa is a type of bacteria that can cause infections in the blood, lungs, and occasionally other parts of the body. These infections are especially common in health care settings, which often encounter drug-resistant bacteria. According to the Centers for Disease Control and Prevention, there were over 30,000 cases of multi-drug resistant P. aeruginosa infections among hospitalized patients in 2017.
The prevalence of antibiotic-resistant Pseudomonas infections makes them a practical point of focus for phage therapy, a type of treatment method using bacteriophages, or phages, that researchers at the Texas A&M Center for Phage Technology are exploring as an alternative to typical drugs.
Zeng and Zhang, codirectors at the center along with Jason Gill, associate professor in the animal science department, are exploring the usefulness of phages, even beyond phage therapy, by diving into the structures and mechanisms at play.
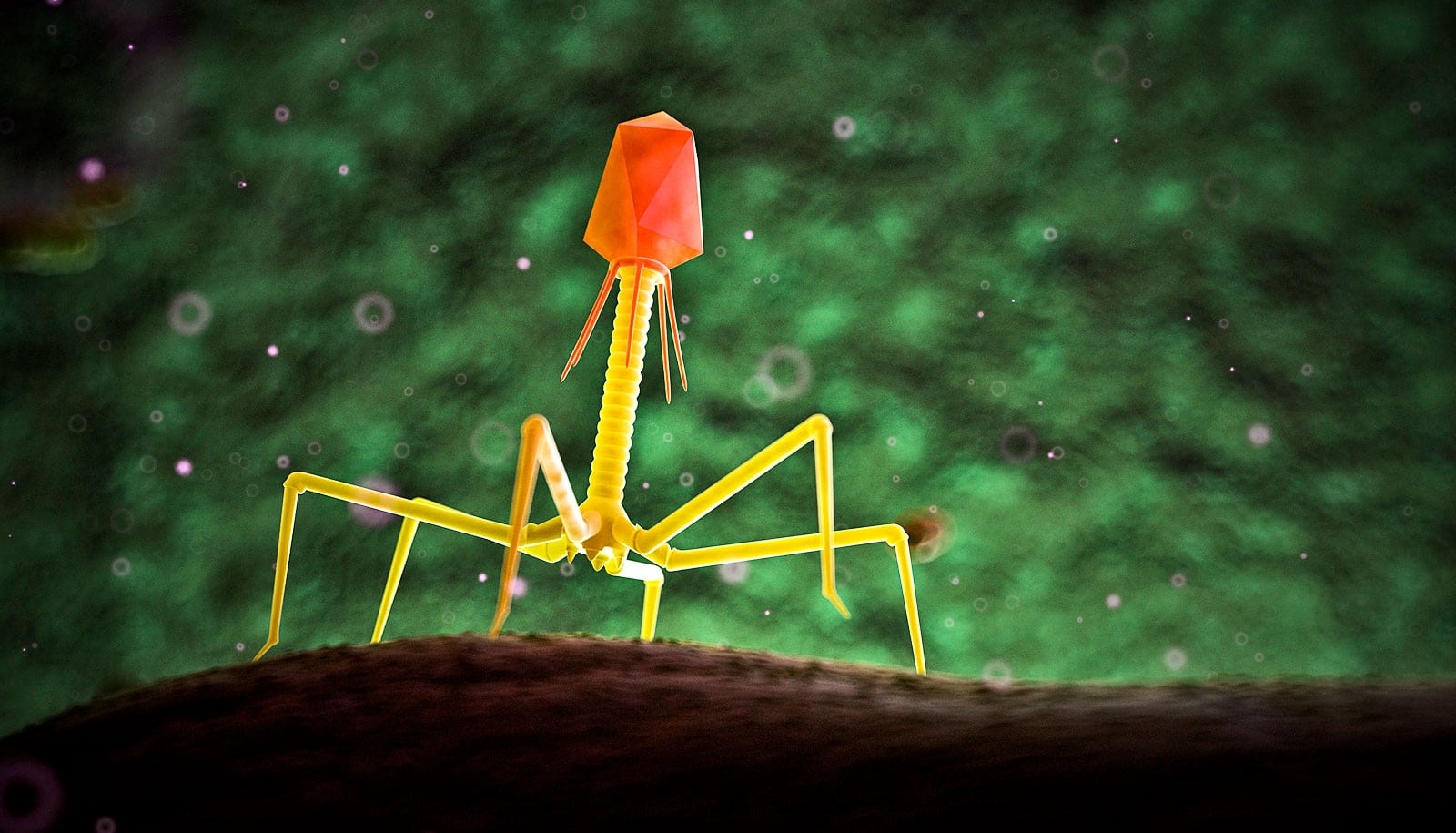
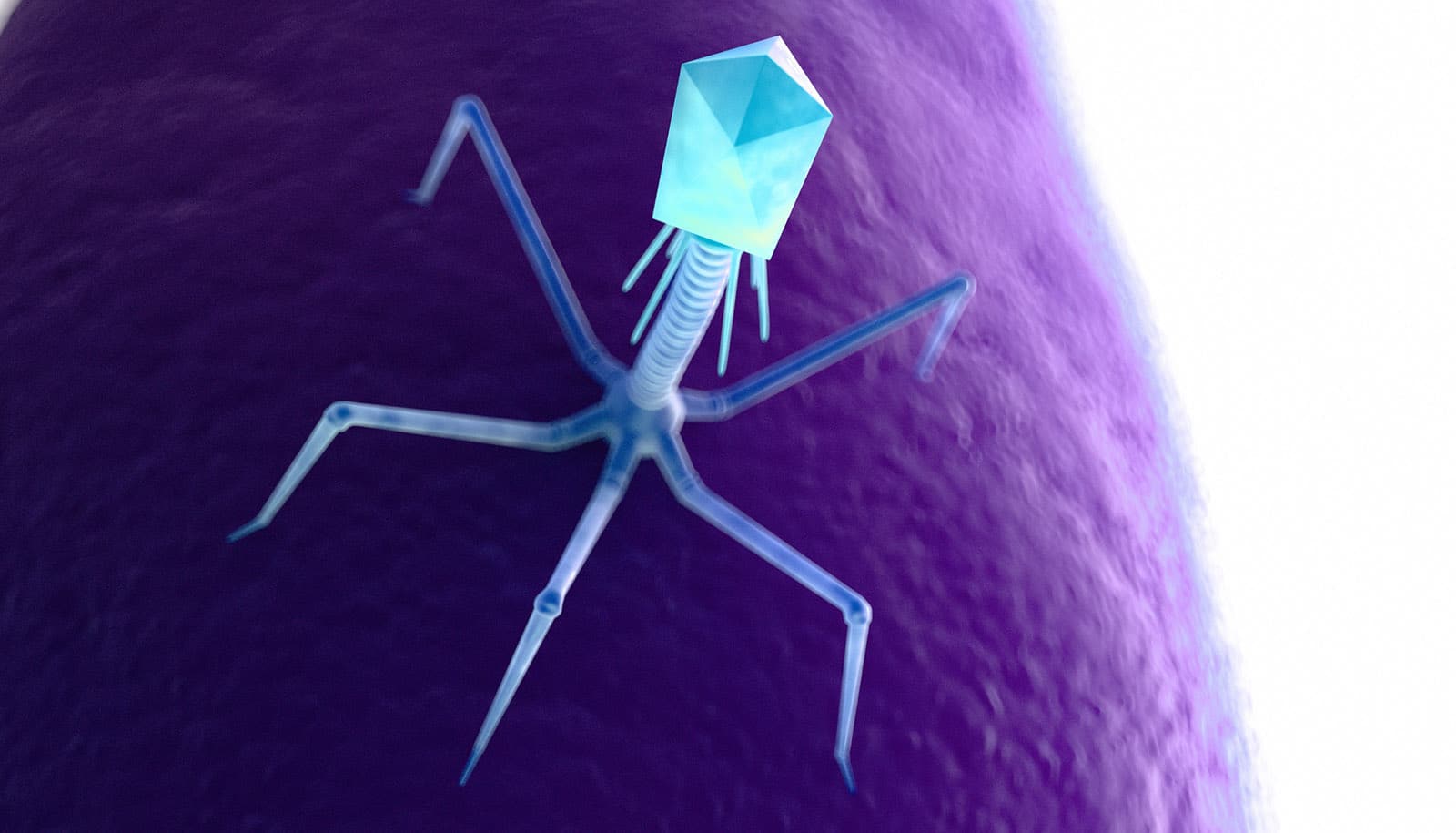
One of the factors that allows P. aeruginosa to transmit antimicrobial-resistant genes among each other, as well as move around and create difficult-to-treat structures called biofilms, is an appendage called a pilus, named after the Latin word for spear. These cylindrical structures extend from the surface of bacteria.
Some phages make use of bacterial pili by attaching to them and allowing bacteria to reel the phage to the surface, where the phage can start infecting the bacteria.
The researchers studied this process step by step using fluorescence microscopy, cryogenic-electron microscopy, and computational modeling. They observed how a phage called PP7 infects P. aeruginosa by attaching to the pilus, which then retracts and pulls the phage to the cell surface.
At the point of entry for the virus, the pilus bends and snaps off, and the loss of the pilus makes P. aeruginosa much less capable of infecting its own host.
Giving the immune system a fighting chance
This work is a continuation of previous research published in 2020, when Zeng’s team found a phage that can similarly break off the pili of E. coli cells, preventing the bacteria from sharing genes among each other—a common way that antibiotic resistance spreads.
The new study is part of the team’s recent suite of research studies. Last month, they published findings in Nature Communications on the interaction between another genus of bacteria, Acinetobacter, and a phage that infects it. Another study, expected to be published next month, will cover a third genus of bacteria and additional phage.
The team’s progress in determining precise protein structures and molecular interactions has been made possible with AgriLife Research’s new cryo-electron microscope, which opened at Texas A&M at the end of 2022 and can resolve structures at the atomic level.
“In our earlier study on E. coli, we did not really explore much about the mechanism,” Zeng says. “In our study of Pseudomonas, we were able to explain much more about what exactly is going on, including the force and speed of pilus detachment, and understand why and how this happens.”
The implications of this ongoing research could prove to be important in treating antimicrobial infections. Zhang says doctors wouldn’t need to use phages to kill the bacteria—as is done in phage therapy—but could simply allow the viruses to disarm the bacteria, which may give the immune system the chance to fight the infection on its own or allow doctors to treat patients with lower doses of antibiotics.
“If you simply kill the bacteria, you break the cells, and they’re going to release toxic material from inside the cell into the host,” Zhang says. “Our approach is to use a particular type of phage that disarms the bacteria. We remove their ability to exchange drug-resistance genes or to move around by breaking off this appendage.”
The team says they will continue looking for similar instances of phages dampening the virulence of pathogenic bacteria.
“We’re taking a synergistic approach,” Zhang says. “We’re trying to understand a universal mechanism for this type of phage and how they’re capable of affecting other types of bacteria. That’s the overall aim of our collaborative effort: to try to tackle the problem of multi-drug resistant bacteria.”
Texas A&M graduate students Jirapat Thongchol and Zihao Yu are the paper’s lead authors. Additional coauthors are from Texas A&M, Princeton University, and the Albert Einstein College of Medicine.
Source: Ashley Vargo for Texas A&M University