Researchers have shown they can modify a “PARP inhibitor” drug to boost its ability to kill cancer cells.
The prospective PARP inhibitor drug has struggled to show effectiveness in clinical trials against cancers, but the modification could change that.
The team also showed they can tune PARP inhibitor compounds in the opposite way so that they inhibit PARP-1 enzymes without killing cells. That may make this class of drugs more useful for treating heart disease and other non-cancer conditions where inhibiting PARP-1 is the goal.
“We can now use this new understanding of how PARP inhibitors work to design compounds that are better tailored for specific conditions such as cancers vs. heart disease,” says senior author Ben Black, a professor of biochemistry and biophysics and co-director of the Penn Center for Genome Integrity at the Perelman School of Medicine at the University of Pennsylvania.
PARP-1 is a DNA-repair enzyme that becomes particularly important for cell survival when other major DNA-repair factors such as BRCA proteins are missing. The US Food and Drug Administration has approved four PARP inhibitors so far, and researchers consider them especially promising as treatments for cancers driven by BRCA gene mutations.
Tumor cells that BRCA mutations drive typically lack any BRCA-based DNA-repair capability, and their exposure to a PARP inhibitor further degrades their ability to fix DNA breaks, making the cells much more likely to die. PARP inhibitors have been shown to improve cancer patient outcomes when used alone or in combination with therapies such as chemo and radiation that induce DNA damage.
Despite promising clinical results for several PARP-1 inhibitors, a mystery has surrounded this drug class. All of these compounds bind tightly to the active site of the PARP-1 enzyme and thus all should inhibit the enzyme very effectively—yet only some of these compounds show potency at killing tumor cells, while others don’t.
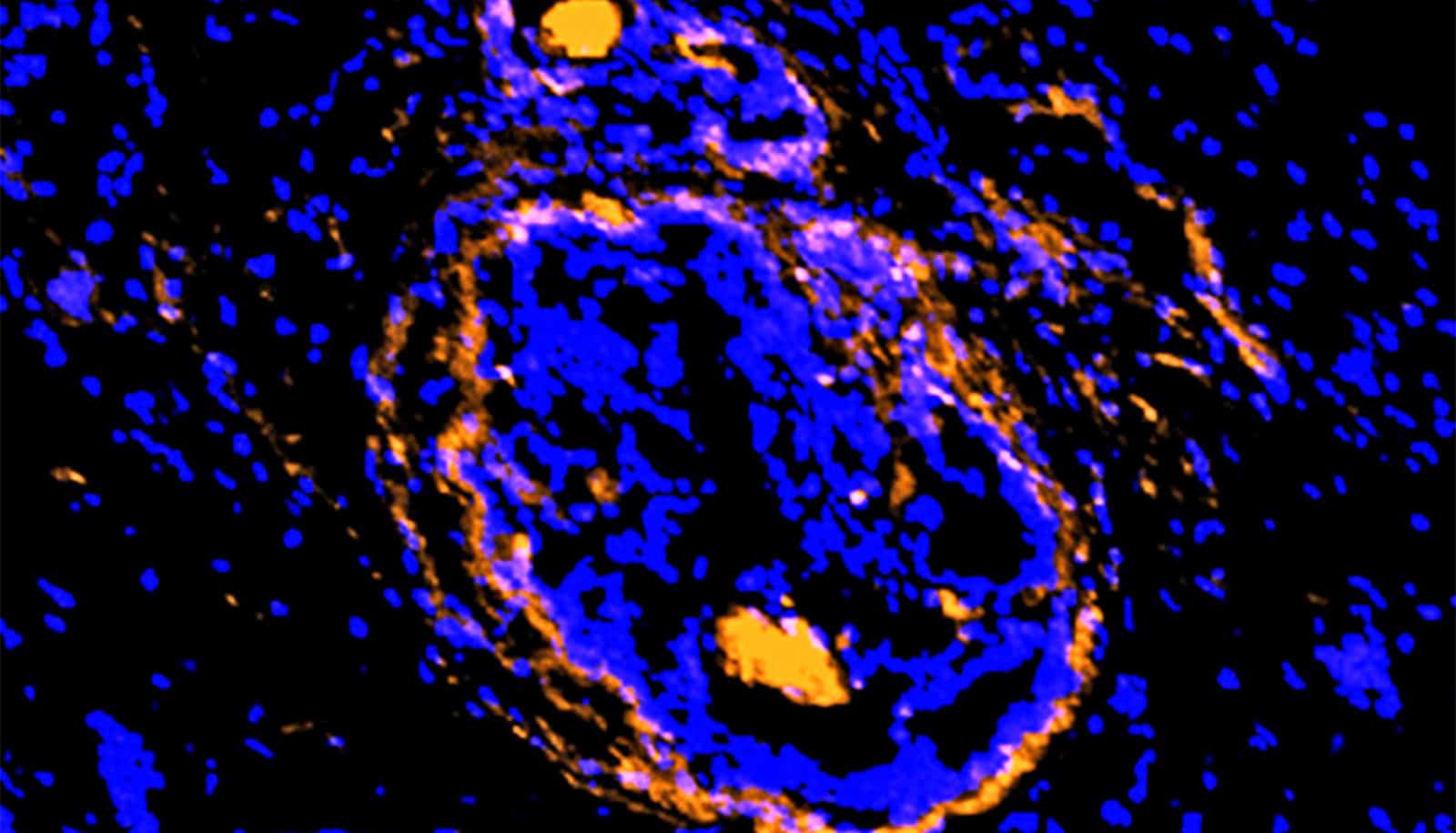
In recent years, scientists have found increasing evidence that PARP inhibitors kill cancer cells not just by inhibiting PARP-1 activity, but also by somehow trapping PARP-1 enzymes on the DNA breaks they are attempting to fix.
Keeping PARP-1 enzymes stuck to a cell’s DNA effectively kills the cell when it attempts to divide—and cancer cells divide relatively frequently. The idea that PARP inhibitors vary in their abilities to “trap” PARP-1 enzymes on DNA has emerged as a potential explanation for these compounds’ variable cancer-killing effects.
In the new study, Black and his team used sophisticated and sensitive techniques to show that PARP inhibitors bind to the PARP-1 enzyme in ways that weaken or strengthen the enzyme’s attachment to DNA breaks. These techniques, which include atomic level structural determination and probing the dynamics of the amide protons of the backbone of PARP-1, go beyond what previous research has done to understand how PARP inhibitors actually work.
Veliparib, a PARP-1 inhibitor that has puzzled pharmaceutical scientists with its failure in recent clinical trials against breast and lung cancers, turns out to weaken PARP-1’s grip on DNA, which in principle makes it easier for a veliparib-treated tumor cell to survive.
The team showed, however, that they could chemically modify veliparib to greatly boost its ability to trap PARP-1 on DNA. This in turn greatly boosted its cancer-cell-killing effects in experiments with different types of cancer cell.
“It was clear that the increased potency of the new compound relative to unmodified veliparib is due to its increased ability to keep PARP-1 bound to DNA breaks,” Black says.
The work greatly clarifies the complex interaction between PARP-1 inhibitors and the PARP-1 enzyme, and shows how variations in this interaction correspond to different cell-killing effects.
In principle, Black notes, researchers can now use this improved understanding to not only design more potent anticancer PARP-1 inhibitors, but also to design PARP-1 inhibitors that don’t kill cells by trapping PARP-1 on DNA.
The latter could be useful in treating inflammation, heart disease, stroke, and other conditions that have been shown to involve excessive PARP-1 activity, potentially including COVID-19.
Support for the work came from the Canadian Institute of Health Research, the US National Institutes of Health, a Basser Center for BRCA Award, the Department of Pharmaceutical Sciences, and seed grant program of St. John’s University, the Breast Cancer Now charity, and Cancer Research UK.
Source: Penn