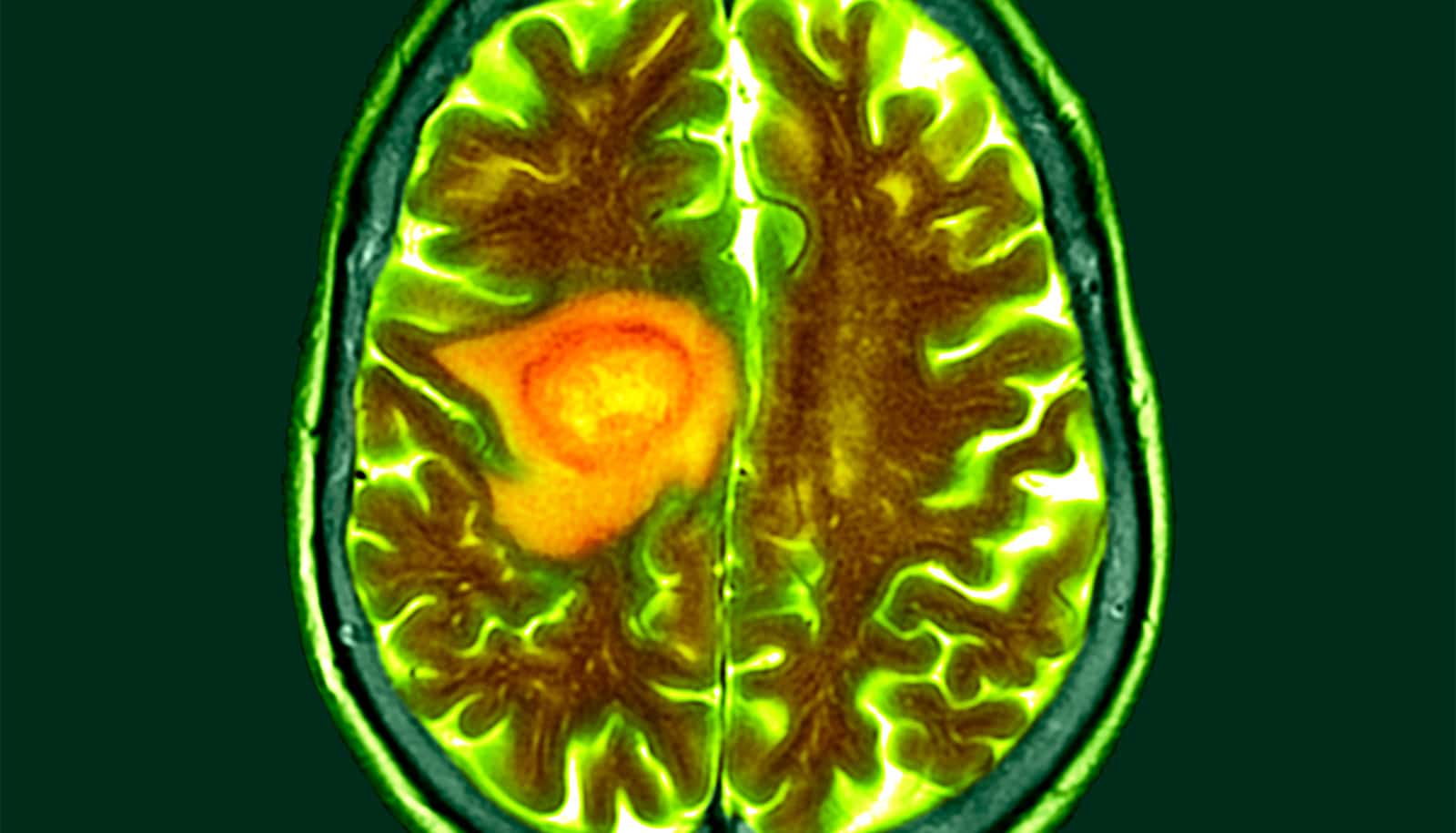
Researchers have developed a nanoparticle to take a chemotherapy drug into fast growing, aggressive brain tumors.
The silica nanoparticle can be loaded with temozolomide, a small molecule drug used to treat glioblastoma brain tumors, the researchers say.
“This chemotherapy drug has limitations—it t doesn’t stay in the blood for very long, it can be pushed out of the brain, and it doesn’t have high penetration from blood into the brain,” says Taskeen Janjua, from the School of Pharmacy at the University of Queensland.
“To make the drug more effective, we developed an ultra-small, large pore nanoparticle to help it move through the blood-brain barrier and penetrate the tumor while also reducing unwanted patient side effects.
“This strategy could be a more effective way to treat brain cancer and prevent it from coming back,” Janjua says.
The nanoparticles are one billionth of a meter in size.
The researchers tested the nanoparticle delivery using 3D spheroids, multi-cellular structures created to mimic the brain tumor cell responses and interactions.
The study results showed that in mice, the nanoparticles successfully accumulated in the brain within a few hours without any negative effects on vital organs.
Brain cancer affects thousands of people every year and the chances of surviving at least five years is less than 23%.
Cancer Australia data showed it was the ninth most common cause of cancer death in Australia in 2020.
While there is still more research to be done, the results are promising for people with brain cancer, says coauthor associate professor Amirali Popat.
“This innovative drug delivery system has the potential to improve the effectiveness of brain cancer treatment and could lead to new and better treatments for this devastating disease,” Popat says.
“This preclinical research will accelerate future clinical development of a promising health technology and further the goal of improving outcomes for patients with brain cancer.”
The study is published in the Journal of Controlled Release. Additional coauthors are from the University of New South Wales and the University of Queensland.
Source: University of Queensland