Researchers have completed the most comprehensive study of whole cancer genomes to date.
The work significantly improves our fundamental understanding of cancer and signposts new directions for its diagnosis and treatment, the researchers report.
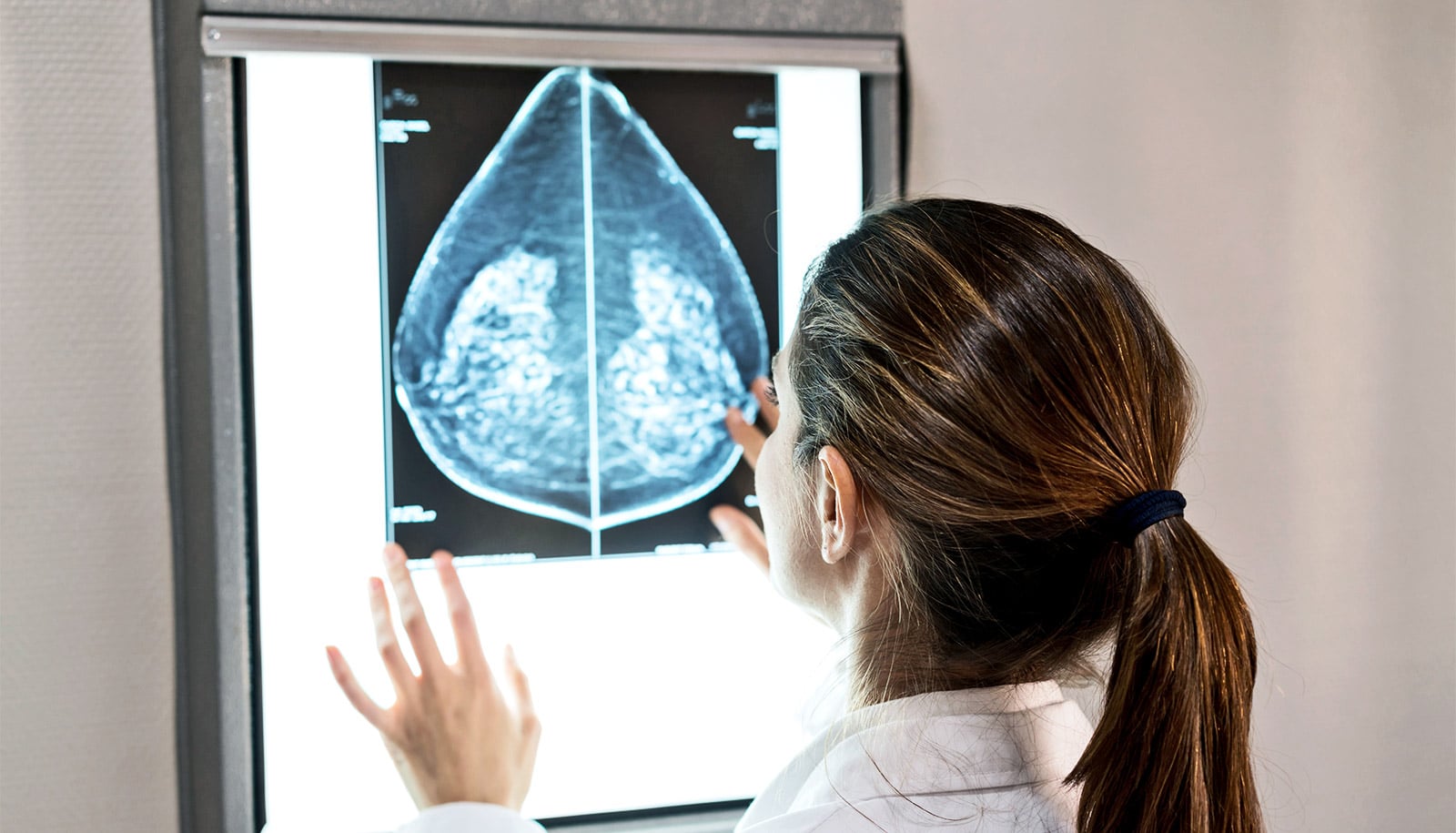
For the new analysis in the journal Nature, more than 700 researchers examined more than 2,600 samples from 38 cancer types. The cancers range from common ones like colorectal and breast cancers to rare cancer types including pancreatic and brain cancers.
This analysis has enabled researchers to create the first complete atlas of genomes to compare the cancers and find the common mutations between them.
The Pan Cancer Analysis of Whole Genomes or the Pan-Cancer Project (PCAWG) created the atlas. PCAWG is a collaboration between groups from the International Cancer Genome Consortium who agreed to put thousands of sets of patient genome data together and reanalyze these samples using cloud computing.
The mutations have all been combined into a sort of catalogue. The catalogue, which is already available online, allows doctors and researchers from all over the world to look things up, consult with, and find information about the cancer of a given patient.
Mapping driver mutations
“Most previous major studies have focused on the protein coding 2% of the genome. We have studied and analyzed the whole genome, and our analyses of mutations that are affecting cancer genes have enabled us to genetically explain 95% of the cancer occurrences we have studied by means of mutations,” says coauthor Joachim Weischenfeldt, associate professor at the Biotech Research & Innovation Centre at the University of Copenhagen and the Finsen Laboratory at Rigshospitalet.
“So, if you know which mutations have caused cancer, the so-called driver mutations, you will be able to better tailor a treatment with the most suitable drugs or design new drugs against the cancer. Precision medicine is completely dependent on the mapping of driver mutations in each cancer, in relation to diagnosis, prognosis, and improved treatment,” says coauthor Jakob Skou Pedersen, a professor at the Bioinformatics Research Centre and in the clinical medicine department at Aarhus University and Aarhus University Hospital.
Researchers found on average any given tumor has four to five key mutations—changes to the genetic blueprint—that are responsible for driving that disease. Those mutations can vary a great deal for each cancer type.
Previously researchers were aware of one or two drivers. Researchers say understanding that number and realizing the complexity in each patient is an important step in working out where else to look when diagnosing cancer patients.
“It is quite surprising that almost all of them have the same number of driver mutations. However, it is consistent with theories that a cancerous tumor needs to change a certain number of mechanisms in the cell before things start to go wrong,” says Pedersen.
This atlas provides a solid foundation for understanding which genes and which pathways may be damaged in each cancer type, says Sean Grimmond, chair in cancer medicine at the University of Melbourne.
“This research will help identify what types of genetic test are needed for each cancer type—filling in potential existing gaps that we did not even know were there,” Grimmond says. “It demonstrates better than ever before how similar damage can cause cancer in different tissues—implications mean that for example a breast cancer drug could be effectively used to treat an esophageal cancer.”
The atlas also identifies patterns of damage across various cancer types, which provides insight for challenging cancers where the tissue of origin is unknown.
“If we don’t understand where a cancer comes from, we can’t even rely on traditional clinical approaches to treatment,” Grimmond says.
Untangling the cancer genome for better treatment
Having a harmonized dataset enables international researchers to learn from one cancer treatment and applies those findings to another using a cloud computing portal.
The researchers say further research with much larger datasets is required to move precision medicine toward becoming a reality.
“This work is helping to answer a long-standing medical difficulty, why two patients with what appear to be the same cancer can have very different outcomes to the same drug treatment,” says Peter Campbell, member of the Pan-Cancer Project steering committee and head of cancer, aging, and somatic mutation at the Wellcome Sanger Institute in the UK.
“We show that the reasons for these different behaviors are written in the DNA. The genome of each patient’s cancer is unique, but there are a finite set of recurring patterns, so with large enough studies we can identify all these patterns to optimize diagnosis and treatment,” Campbell says.
“Cancer is a genetic disease, and the type of mutations is often more important than where the cancer originates in the body. This means that we need to think of cancer not just as a tissue-specific disease, but rather look at it based on genetics and the mutations it has,” says Weischenfeldt.
“For example, we may have a type of breast cancer and prostate cancer where the driver mutations are similar. This means that the patient with prostate cancer may benefit from the same treatment as the one you would give the breast cancer patient, because the two types share an important driver mutation.”