Though challenges remain in fighting the spread of coronavirus, the United States government has tools ready to face a potential pandemic, an expert explains.
“About 80% of people with COVID-19 have only mild symptoms, and the latest data suggest about 98% survive.”
The CDC issued a statement this week stating that “Americans should brace for the likelihood that the coronavirus will spread to communities in the US” and to “prepare for the expectation that this might be bad.”
With estimates of infection worldwide now exceeding 80,000—and about 2,600 now dead—what are the legal tools in place for the US and world to deal with a pandemic?
Here, Michelle Mello, professor of law and professor of health research and policy in the Stanford University School of Medicine, discusses the virus and the development of policy to contain its spread:
How carefully is the US tracking the coronavirus within our borders? There is some speculation that the virus has been under-reported in the US because the diagnostic kit sent to states was flawed.
There have been problems with both the test itself and its dissemination to labs across the US, and it’s possible that these circumstances may have led to missed diagnoses. We know they have led to late diagnoses in at least a few cases.
The problem with the test itself had to do with one of its ingredients and is now solved. The other problem was that originally, labs didn’t have permission to perform the text locally, which slowed things down.
That has also been addressed: the number of labs performing tests will exceed 90 by next week.
What are the other challenges to getting accurate estimates about the number of infected?
A remaining challenge is who should get the test. COVID-19 symptoms look a lot like those of other respiratory illnesses. To date, the criteria for who gets tested have been quite narrow, but the CDC and state and local health departments are actively working on whether and how to tweak those criteria.
Although there are probably undetected cases out there, it’s important to keep things in perspective. This infographic using data through late February shows that this season we’ve had about 29 million cases of seasonal influenza, resulting in at least 16,000 deaths.
We’ve had about 60 cases of COVID-19 and 0 deaths. About 80% of people with COVID-19 have only mild symptoms, and the latest data suggest about 98% survive.
Do we have the legal and regulatory tools in place to deal with a pandemic here in the US?
Yes. For the past two decades the federal government, the state, and the international community have been updating and augmenting the web of laws that authorize government action in response to outbreaks of infectious disease and other public health emergencies.
Here in the US, both the states and the federal government have broad, everyday powers to intervene to stop disease transmission through measures such as isolation, quarantine, and mandatory vaccination. Then there are a suite of special powers that are triggered when a designated official declares an emergency, and they are even broader.
In addition to coercive powers like quarantine, at the federal level they include powers to release strategic resources, such as stockpiled medical supplies and pots of money, that have been socked away. Congress can also appropriate additional resources to be directed to outbreak response, and the president has some power to reallocate money within health agencies’ budgets.
How about global cooperation in halting the spread of this virus?
Globally, each country is in charge of its own response. But they have pledged cooperation through the International Health Regulations. Adopted in 2005, the IHR are an agreement among 196 nations to ensure that they have capacity to detect and report public health events in their own countries and to adhere to certain measures at borders to limit the spread of disease across countries.
These are voluntary commitments and nations have different capacities to implement them, but the legal framework is in place. Adherence is facilitated when wealthier countries provide aid to low-resource countries to help them carry out these functions.
How closely are countries working together to develop policy to understand this virus and to contain its spread—and to develop better testing and a vaccine? Who is leading that effort?
Cooperation evidently got off to a rocky start in terms of the degree of transparency the Chinese government practiced when it first became aware of the problem. But on the scientific front, things have been very encouraging.
The World Health Organization has led efforts to assess what we know and don’t know, set research priorities, and identify funding. WHO has also kept the world informed about the global march of the virus. Researchers, mostly within China, have vigorously studied and published data on the numbers of cases, hospitalizations, and deaths, and other researchers have swiftly built models projecting the course of the epidemic, which medical journals have made public with amazing speed. WHO and other organizations are also facilitating coordination on matters like travel and tourism.
What weaknesses in the government’s ability to control dangerous health threats is this virus highlighting?
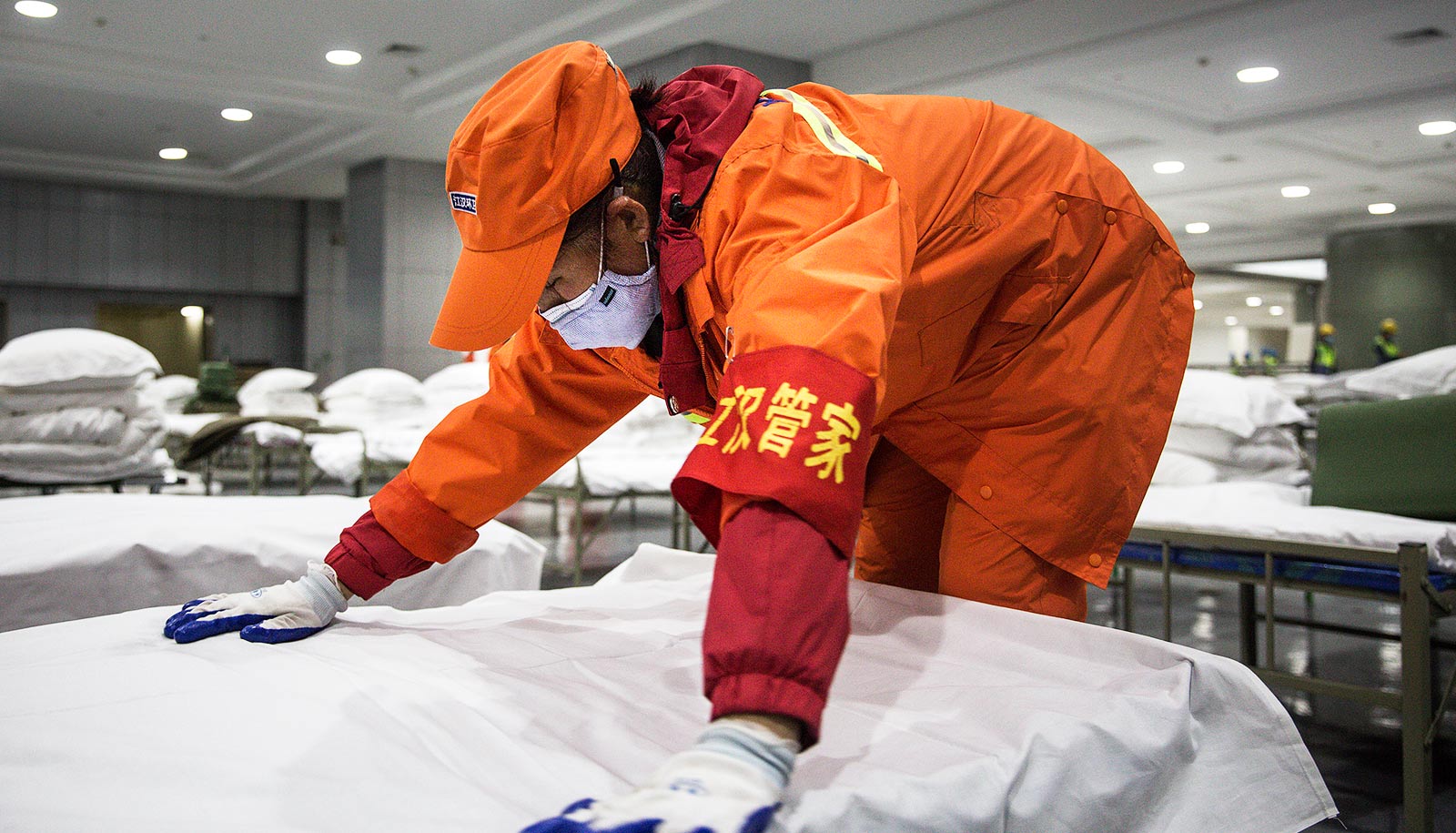
I see two. First, the Wuhan quarantine dramatically illustrated the challenges of maintaining a mass quarantine over an extended period of time. What the government did there is highly unusual; typically, isolation and quarantine orders are far narrower and better tailored to the people who have actually been exposed to the virus. It’s virtually impossible to maintain a mass quarantine for a long period because critical supplies will run out and social unrest will grow.
A scenario like that in the US is highly unlikely, but it’s striking to me that there has been so little discussion of how to make it feasible for people to stay at home for extended periods of time, whether under a government order or voluntarily. How can workers be kept afloat economically when they lose pay? How can continuity be maintained in children’s education and in supplies of necessities? When we need to ask people to self-isolate, there should be reciprocity—expressions of support and caring that make it feasible for them to do the right thing.
Second, our government has a short attention span. We have an outbreak of a novel virus, we throw a lot of resources at it, it abates, and then we pull the resources back and use them for something else—before our work is done. As a result, promising research to bring vaccines and therapeutics to market isn’t followed through on; capacity-building in low-resource countries (such as building hospitals and testing facilities) stops; and we’re no better prepared for the next outbreak than we were for the last one.
For example, as soon as the 2014 Ebola outbreak subsided, we diverted resources earmarked for Ebola response to Zika virus. It’s entirely predictable that outbreaks will recur, so we need to keep working on prevention and response planning during the inter-pandemic period.
Is there anything else you’d like to add?
The CDC has a helpful webpage with FAQs about COVID-19, and it’s far more informative than the lurid coverage on TV news. I flew cross country yesterday and can report that there were many more people wearing masks (not recommended) than washing their hands properly (recommended)! A little refresher on how to prevent the spread of respiratory illnesses is the best medicine right now.
Source: Stanford University