Emphysema is a long-term and devastating lung disease. As it progresses, the body’s own inflammatory enzymes slowly digest and destroy alveoli, the delicate sacs where oxygen from air is transferred to the bloodstream.
The damaged alveoli form large holes in lung tissue that impair gas exchange in the rest of the organ, leading to shortness of breath, wheezing, chronic cough, and, eventually, death.
By looking at the disease with engineers’ eyes, researchers have gained insight into how it progresses. A new study, published in PLOS Computational Biology, suggests how mechanical forces operating on a microscopic scale could help predict patient survival and quality of life following treatment.
“In the future, you should be able to optimize treatment for a specific patient,” says Béla Suki, professor of biomedical engineering at Boston University. “Very few computational studies have been able to address quality of life.”
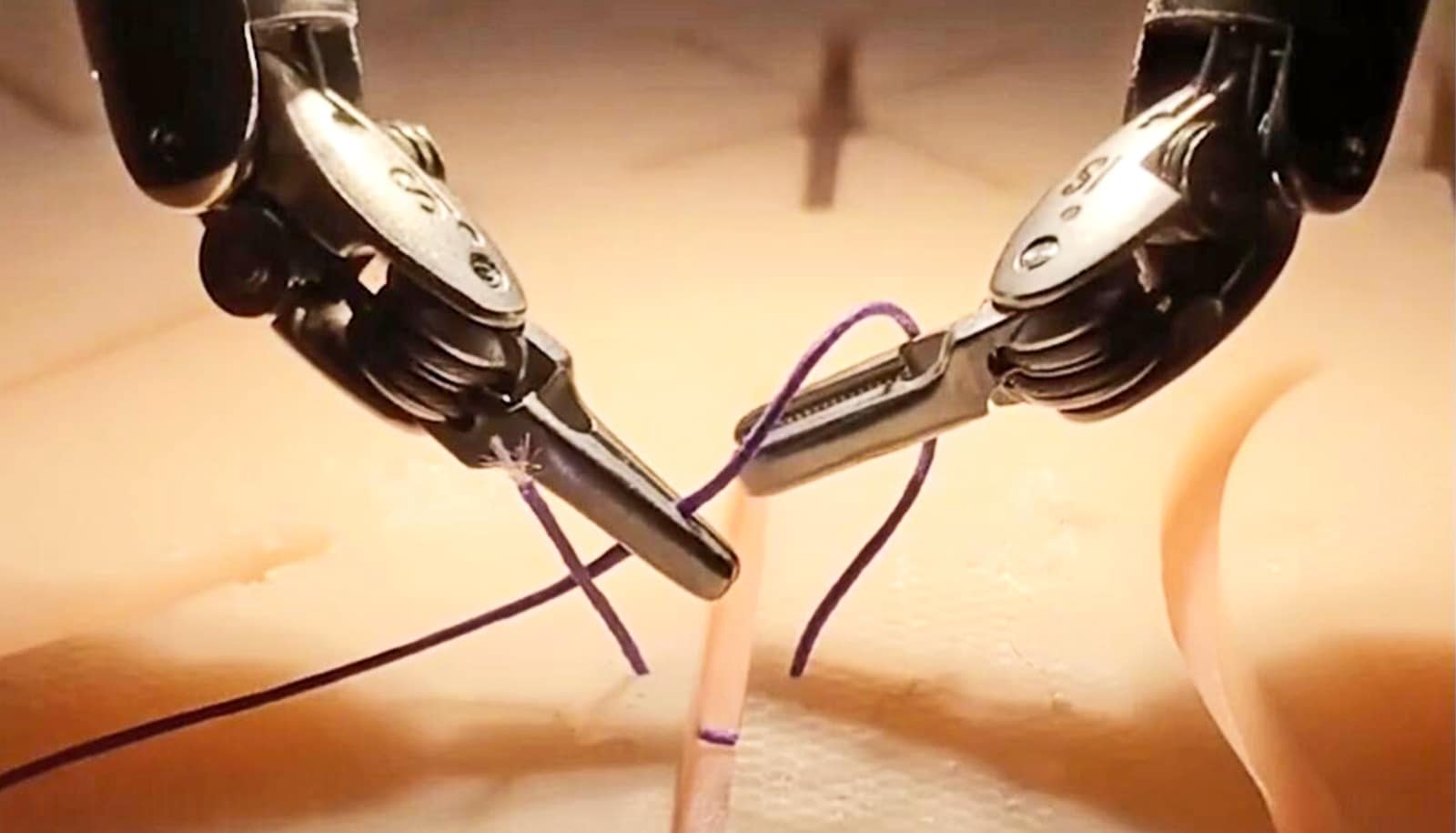
Emphysema has no cure, and for many years the last-ditch treatment for the disease was an invasive surgery called lung volume reduction, in which a surgeon opens a patient’s chest and removes the diseased, inflamed portions of the lung. The surgery gives the remaining healthy lung tissue room to expand and allows the patient to breathe. But the procedure only works in some people, and the effects vary widely among patients.
Oxygen doesn’t benefit everyone with COPD
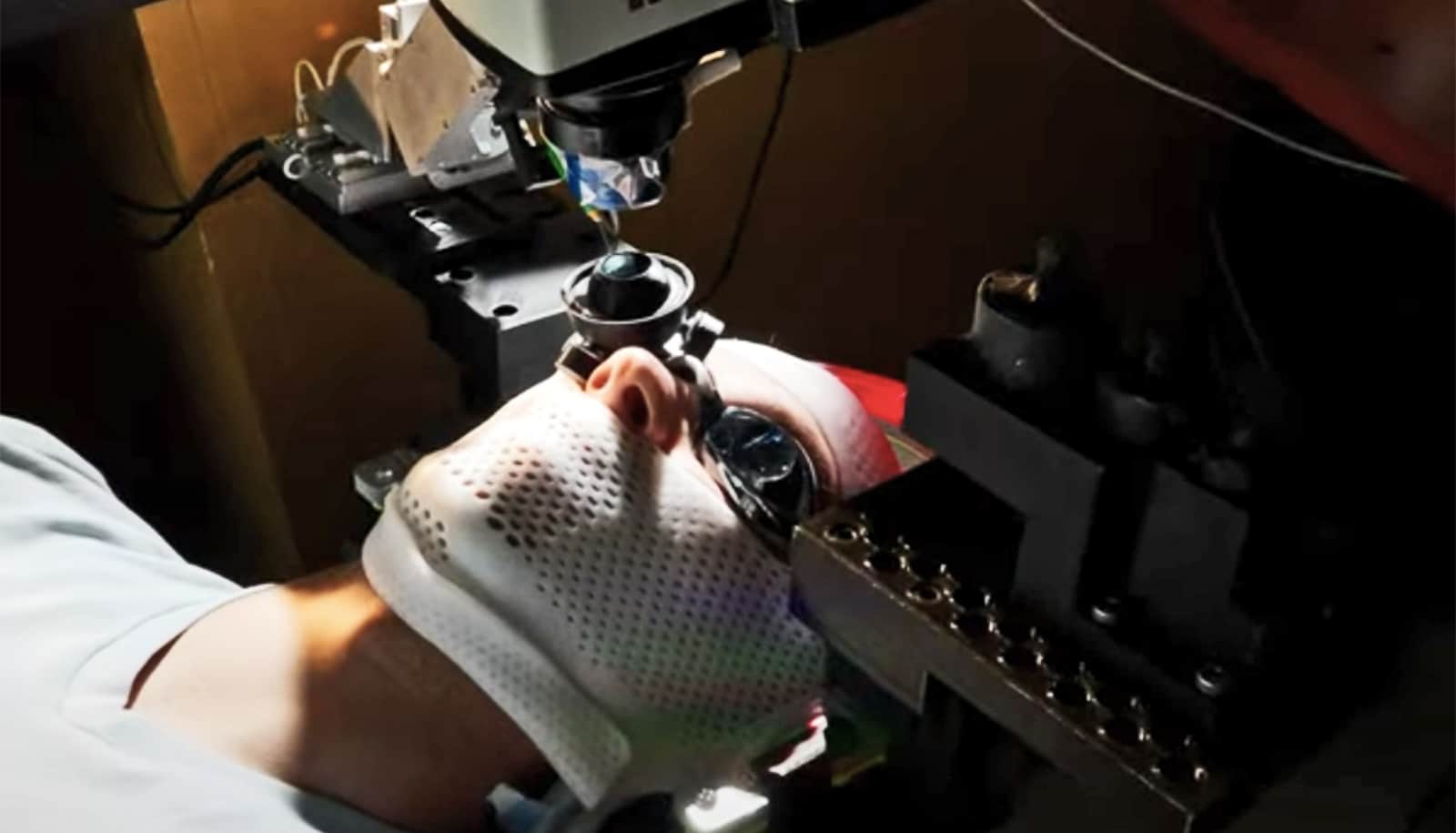
In recent years, surgeons have begun using a less-invasive treatment called bronchoscopic lung volume reduction (bLVR). In this outpatient procedure, a bronchoscope is inserted into a patient’s diseased lung and releases a sealant, or, alternately, a coiled spring, which collapses the diseased tissue, closing gaps and giving the remaining healthy lung tissue room to expand.
Interest in these treatments has grown recently, as the results of clinical trials like REVOLENS, published in JAMA in 2016, showed significant improvement for some patients six months after surgery. But no research has explained why the procedures work better in some patients than others.
“Even if you quit smoking, emphysema keeps progressing, though at a lower rate.”
“There’s been a lot of research, clinical trials. But not much investigation of what’s happening at the microscopic scale,” says Jarred Mondoñedo a School of Medicine MD candidate and lead author of the PLOS Computational Biology study. “That’s where the direction of this research came from. We said, ‘Let’s really find out what’s going on.'”
Simple computer program
The new research builds on previously published results from Suki, who had studied the elastic properties of healthy and diseased lung tissue by actually stretching samples in the lab. One of Suki’s students found, accidentally, that emphysematous tissue broke under surprisingly low strain. This led Suki to further investigate the mechanical forces at work as emphysema progresses.
“Even if you quit smoking, emphysema keeps progressing, though at a lower rate,” says Suki. “The reason is that when something ruptures in the lung, the tension that element carried is going to be distributed around. The other elements will start to carry a little bit higher force, so they are at a higher risk of failure. And that makes a progressive feedback.”
2 chronic lung diseases share gene changes
To better understand this process, the researchers built a simple computer program, called an elastic spring network model, to mimic lungs with emphysema.
“It’s not a super complicated model,” says Mondoñedo, who says it represents the connections and tensions between sections of lung tissue as hexagons of interconnected springs. “We can go through and ‘break’ the springs, and we get a new configuration that represents the progression of emphysema,” he says.
Mondoñedo and Suki ran the computer model in different ways, allowing the emphysema to progress, then “intervening” with various treatment—such as surgery—at different times, then allowing the model to progress further and quantifying the results.
“In the computer, you can play God,” says Suki. “We just do the surgery in the computer, and then we let it evolve, and now it’s easy for us to compare the rate at which things happen.”
They measured a factor called “compliance,” which quantifies the stretchiness of lung tissue. “And we could say that, well, if the compliance reaches such-and-such a value, basically the lung is so much destroyed that the person dies. And then we can predict how long it would take, with or without intervention, and also what your lung function is, how easy it is to breathe.”
Their computer model suggests that bLVR performs as well as, or better than, traditional lung volume reduction surgery, and also suggests a mechanism—force distribution and its relation to lung structure—that explains, for the first time, why this is the case. It also confirms previous findings that the procedures work best for patients who are affected only in specific parts of their lungs, rather than evenly throughout the lung tissue.
The scientists express hope that their model may someday help physicians and patients decide which procedure will work best for each individual.
“If you could take a CT scan of a patient and then somehow fit that data into our network model, you could develop a strategy based on that particular patient, rather than one-size-fits-all,” says Mondoñedo. “In that way I think it could translate into clinics and enhance care.”
Source: Boston University