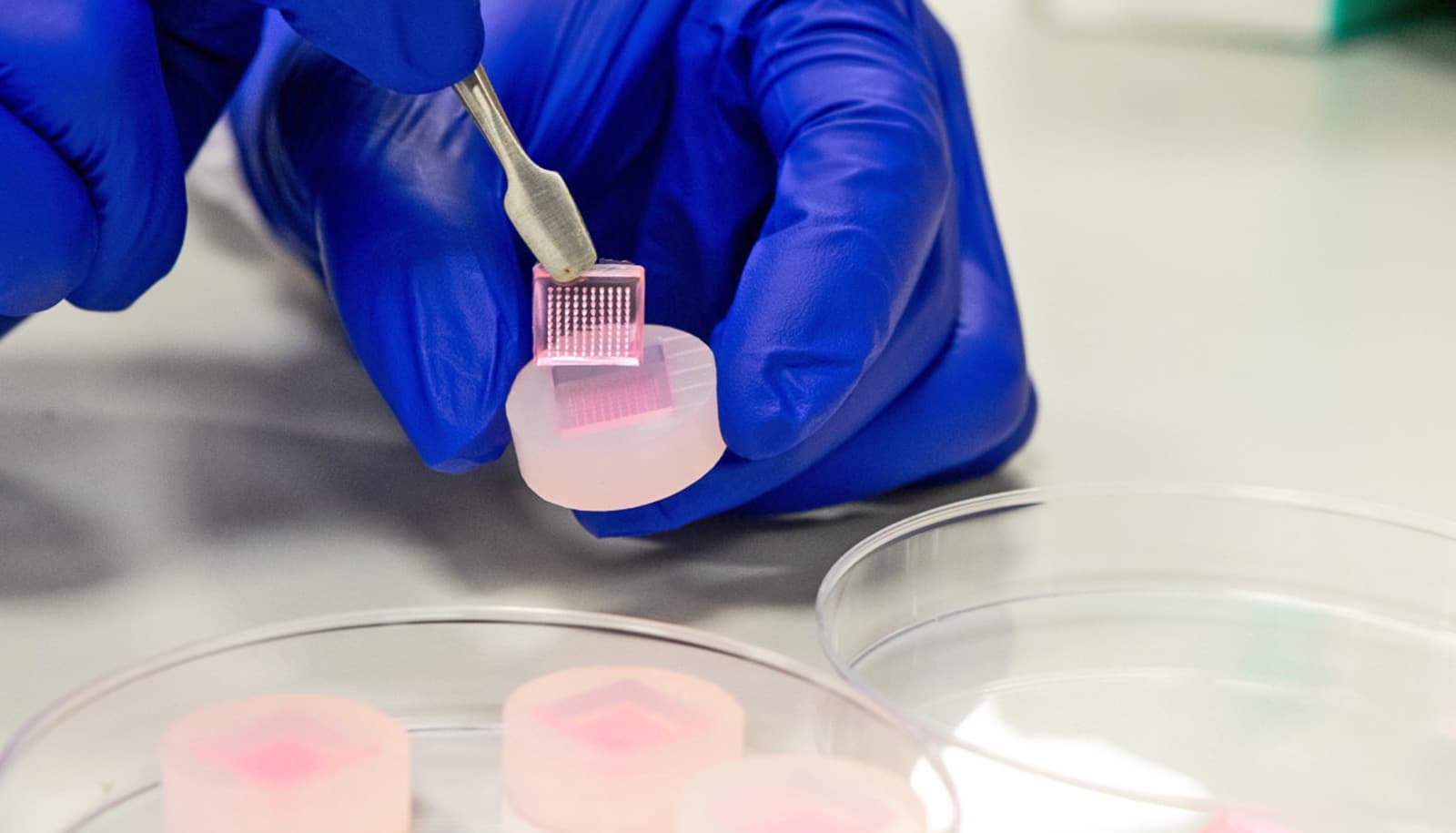
Researchers have incorporated platelet-rich plasma into a bio-ink: a 3D-printed mixture of cells and gel that could eventually be part of skin grafts and regenerative tissue implants.
If injury strikes during their 10-day cruise through the bloodstream, platelets flock toward the scene of a cut or bruise to engage their signature superpower: clotting.
But platelets also release so-called growth factors that help repair soft tissues—blood vessels, skin, muscle, tendons—and recruit other cells to speed the healing process. Those capabilities have made platelet-rich plasma an emerging treatment option for certain joint injuries and post-operative therapies.
“The ultimate goal is to print functional tissue constructs that can be implanted to replace or repair damaged tissues,” says Ali Tamayol, assistant professor of mechanical and materials engineering at the University of Nebraska-Lincoln. “One of the challenges is to create structures that, when implanted in selected tissues or organs after an injury, will release growth factors that initiate the processes essential for healing and regeneration.”
Platelet-rich
Jeremy Ruskin, professor of medicine at Harvard Medical School, worked with colleagues at Massachusetts General Hospital to show that the bio-ink can accommodate an optimal concentration of platelet-rich plasma and dispense its growth factors over several days. And when testing the performance of its platelet-rich ink against a platelet-less counterpart in the lab, the team saw some promising results.
In less than a day, the platelet-rich ink had prompted enough cell migration to cover about 50 percent of an artificial scratch, whereas the platelet-less edition covered just 5 percent. The ink also excelled at calling for reinforcements, encouraging more than twice as many mesenchymal stem cells—which can become muscle, cartilage, or bone—to migrate toward it during a 24-hour span.
Because proper healing depends on adequate blood flow, the researchers likewise tested their ink’s ability to stimulate the reconstruction of blood vessels. They found that vessel-specific cells not only reproduced twice as fast but also organized into vessel-like tubes that were substantially longer and more complex than those formed by the platelet-less ink.
Good gel for 3D printing
Yet those results would mean little if the ink’s primary ingredient—a gelatinous, algae-derived material called alginate—proved resistant to 3D printing or failed to maintain its form. Tamayol and colleagues initially peppered the alginate with calcium chloride to forge bonds among some of the material’s polymer chains, lending it strength without making it too viscous for a 3D printer.
Fake platelets clot blood and then dissolve
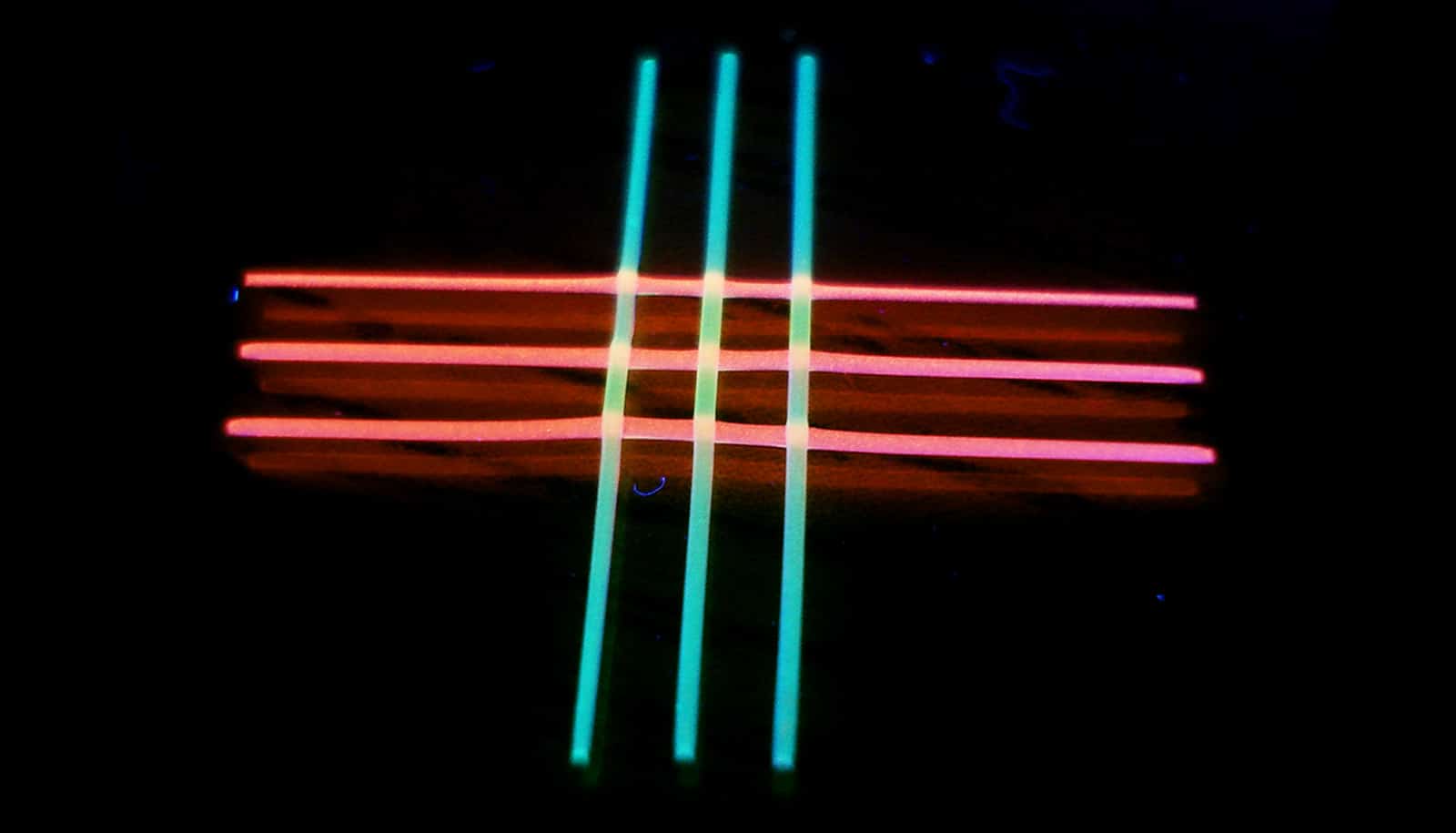
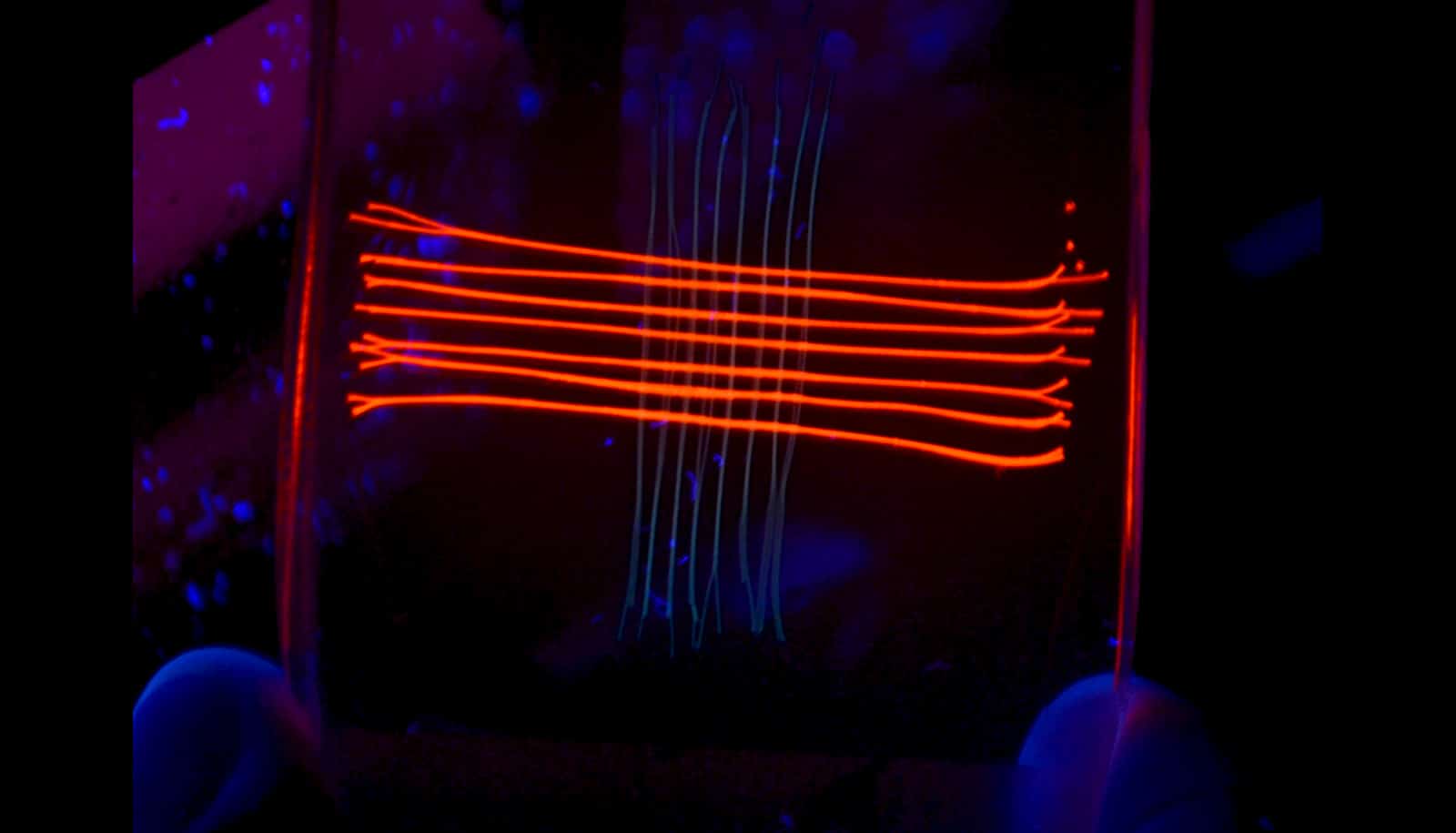
After printing the ink into a desired 3D design—the researchers demonstrated a grid, a tree-like structure, and a serpentine line—they immersed the structure in a calcium chloride solution to further strengthen it. The body also raises calcium levels at injury sites, meaning that it could help reinforce the alginate after implantation, Tamayol says.
Once bio-printing technology has matured, he says, the alginate could be mixed with a patient’s own cells and platelets to minimize the risk of an immune response.
“There is a trend toward using personalized therapies in many areas of medicine,” says Negar Faramarzi, the lead author of the study in Advanced Healthcare Materials. “We tried to incorporate the growth factors in a way that keeps us on track for those personalized therapies.”
The team received support from the National Institutes of Health, the Nebraska Tobacco Settlement, and the Al-Sagri Research Fund at Massachusetts General Hospital.
Source: University of Nebraska-Lincoln