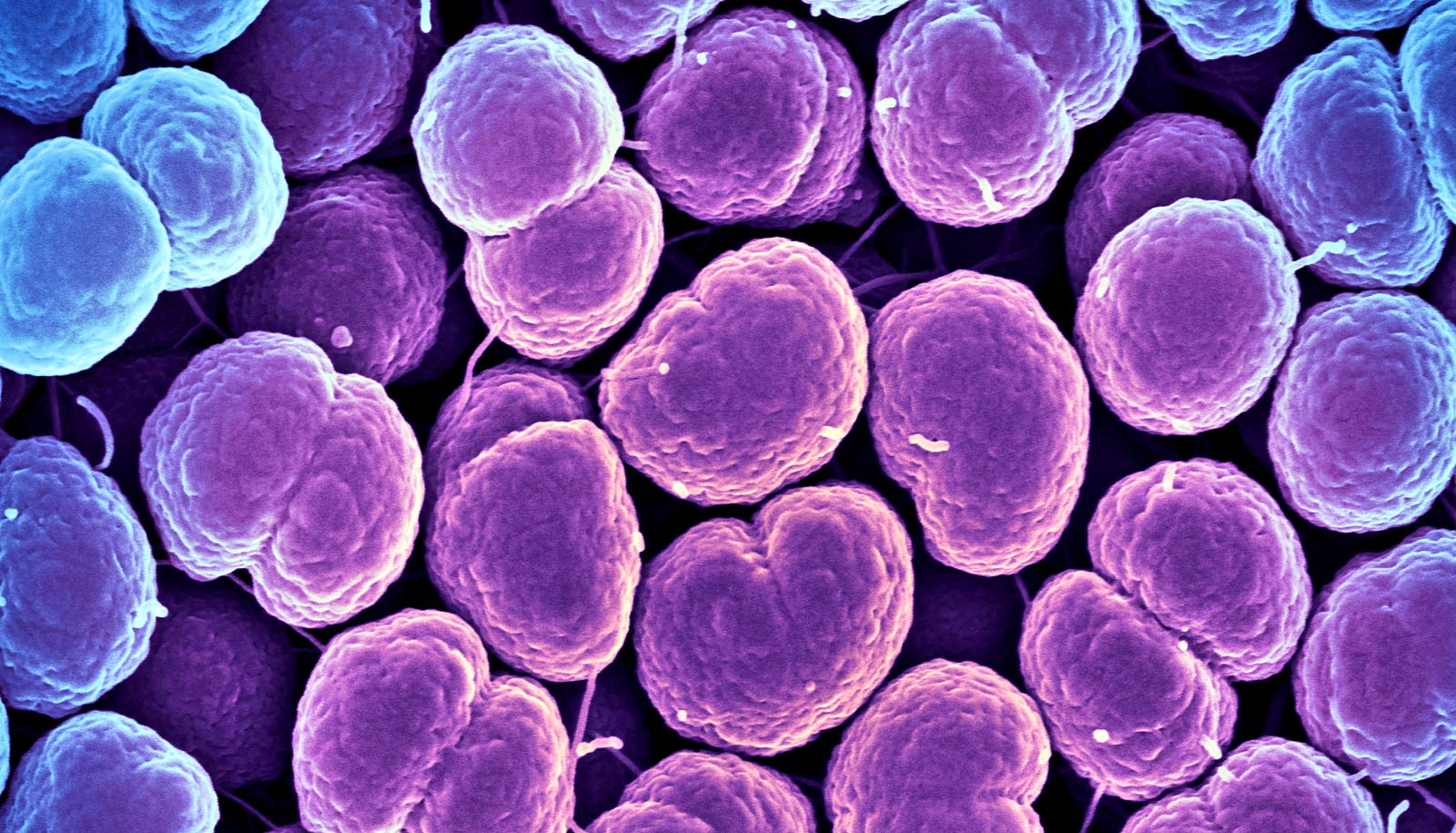
A strain of bacteria found on human skin is becoming resistant to most antibiotics, a new study warns.
When Jean Lee came across a case of an otherwise healthy patient who had become seriously ill from a hospital-acquired infection in 2012, she knew she had to investigate further.
Lee, who was working as an infectious diseases registrar at a Melbourne hospital, became concerned when the patient experienced complications following a relatively simple elective procedure.
“…resistance has got to the point where some of these cases are almost untreatable.”
“He should have been in and out of hospital quickly,” she says. “But instead he contracted a very resistant infection and had to stay in hospital for over two months, followed by rehab.”
It turned out he had contracted Staphylococcus epidermidis (S. epidermidis), one of the most common causes of hospital associated infections.
The strain hasn’t previously been considered a major concern—doctors were more worried about other antibiotic-resistant superbugs like methicillin-resistant Staphylococcus aureus (MRSA)—commonly known as golden staph.
But new research shows that in some parts of Europe, some strains of S. epidermidis are already resistant to all known antibiotics.
“Other bugs are more deadly, and this is a bug we all have on our skin, so I think there’s a perception it’s not quite so bad and that when a patient contracts it we can deal with it,” Lee says. “But we’ve discovered resistance has got to the point where some of these cases are almost untreatable.”
Last line of defense
After discovering her patient’s infection was caused by S. epidermidis, Lee started a six-year project with her consultant and PhD supervisor, Ben Howden, to understand how widespread its resistance is.
The findings appear in Nature Microbiology.
The researchers identified three strains of the bacteria, which have become resistant to the two separate antibiotics currently used to treat infections—rifampicin and vancomycin.
Howden, a clinician and the director of the microbiological diagnostic unit public health laboratory at the Doherty Institute, says this resistance is concerning because vancomycin in particular is used as a last line of defense against infections.
“Current guidelines for these types of infections recommend a combination treatment of rifampicin and vancomycin, which are completely unrelated and should protect against one another,” Howden says.
“But this finding reveals resistance to one antibiotic is causing resistance in the other, raising concerns about current treatment guidelines.
“It has also managed to spread despite the good infection control now in place in hospitals in developed countries, which has helped manage golden staph.”
Resistant strains everywhere
Lee and Howden first established that the resistant strains were present in hospitals in Victoria, and then expanded their search to determine where else they could be found. They looked at hundreds of S. epidermidis cases from 78 institutions in 10 countries around the world and discovered they have spread globally.
“We worked with reference centers in the UK, Europe, and America,” Lee says. “These centers are sent difficult to treat or unusual bugs from individual hospital laboratories. We discovered these three new strains in difficult-to-treat cases in completely unrelated people.
“When we saw the infections exhibiting the same pattern of antibiotic resistance we realized the new resistant strains are everywhere.”
The researchers used the whole genome sequencing technology available at the Doherty Institute to rapidly sequence the bacteria’s whole genetic code.
“This meant we could compare our international samples at a genetic level to see how they were related,” Howden says. “We found the same mutations making bugs very antibiotic resistant in every country we tested.”
Patients tend to contract an S. epidermidis infection when they have a foreign object, like a line to administer drug or a catheter, inserted. Because the bug isn’t particularly virulent, infected patients also tend to be immunocompromised.
“When you break the skin you provide an entry portal for the bug, so an infection usually requires something that doesn’t belong in the body,” Lee says. “The bug creates a protective layer around whatever has been inserted, which allows it to avoid antibiotics and the body’s immune response.”
Intensive care
It is commonly found among patients in intensive care, because they tend to have so many lines inserted, and it is likely this has contributed to the spread of the resistant strains, Howden says.
“Catheters and other implanted devices are frequently impregnated with antibiotics as a strategy to prevent infection, however this approach may be promoting the development of resistance.
“Also, these infections are most prevalent in intensive care, where patients are sickest and strong antibiotics are liberally prescribed, promoting the development of additional resistance.”
While the researchers say it’s likely patients only acquire these new strains of S. epidermidis in hospital environments, they don’t yet know how it is spreading internationally.
“We know what we’re currently doing is just leading to more resistance.”
“Like so many areas of science, this discovery has raised lots of new questions,” Lee says. “One of the most pressing is to work out exactly how the bug is being passed to patients. Knowing the mechanism will help us work out how it is spreading internationally.
“We also need to understand all the clinical outcomes—how much is the antibiotic resistance contributing to poor outcomes and what can be done about it.”
One of the first tasks is to revise treatment guidelines, Howden says.
“We know what we’re currently doing is just leading to more resistance. So, we urgently need to think about what we should be recommending instead,” he says.
“There is an urgent need for an international monitoring system to understand the prevalence and impact of S. epidermidis and to systematically measure antibiotic resistance and infections due to this pathogen.”
Source: University of Melbourne