In order to compensate for lack of ventilators, hospitals have started to convert anesthesia machines into breathing machines.
As COVID-19 cases continue to rise, concern at hospitals about a shortage of personal protective equipment and ventilators that help critically ill patients breathe is on the rise.
Michael McLaughlin, an assistant professor and assistant program director of the Rutgers University Nurse Anesthesia program, has been on the frontlines of the COVID-19 crisis and intubated many COVID-19 patients.
Here he discusses how the anesthesia machine conversion works and how it can help alleviate the ventilator shortage:
What is an anesthesia machine?
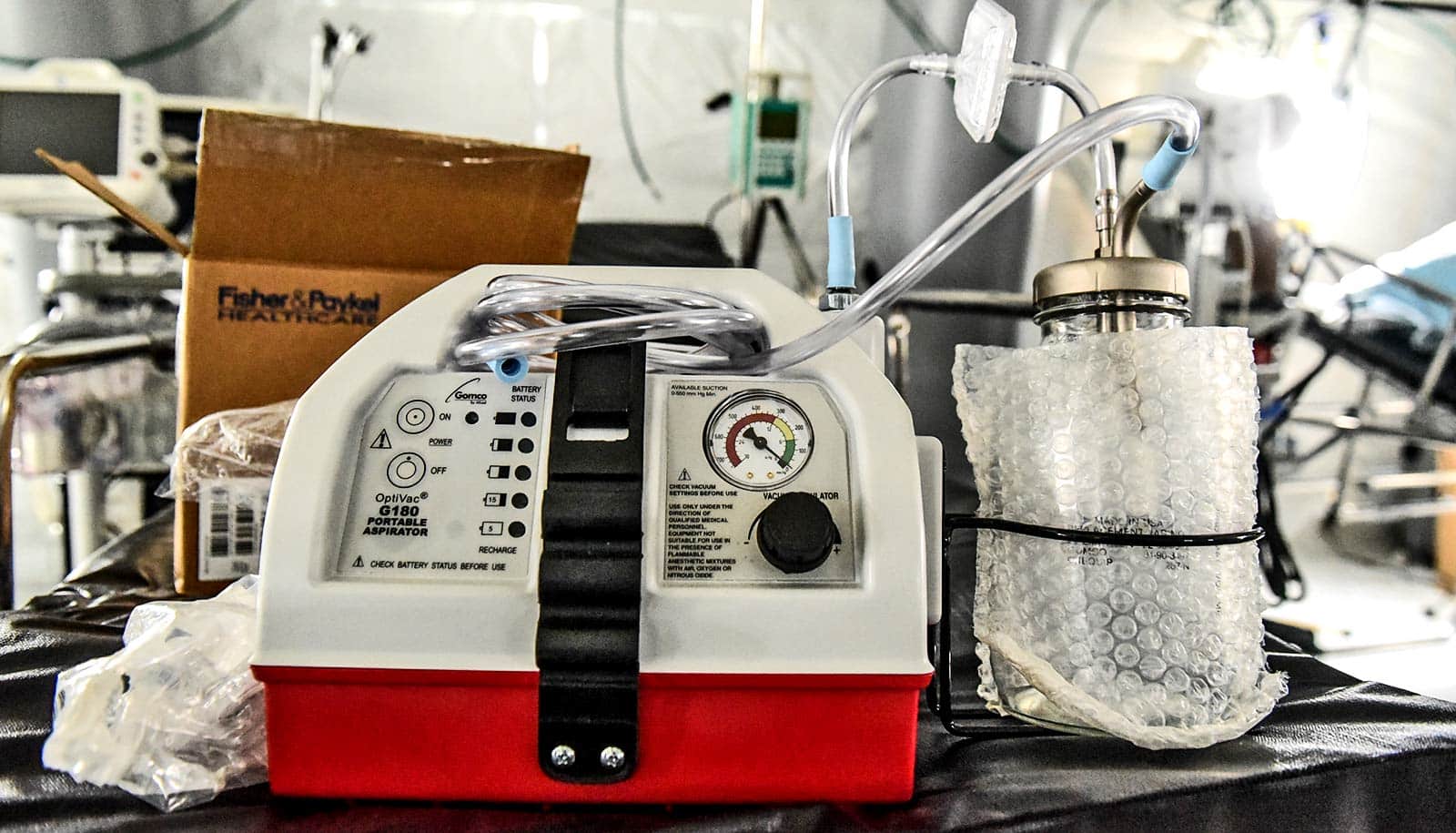
An anesthesia machine is a medical device typically used to administer inhalation anesthesia. It delivers a mix of anesthesia gases and oxygen to patients while also monitoring blood pressure, pulse rate, and temperature.
Anesthesia machines consist of flowmeters, vaporizers, CO2 absorbers, sources of compressed gases, and a mechanical ventilator.
How quickly and easily can an anesthesia machine be converted to a ventilator?
Anesthesia machines can be converted to ventilators in a matter of minutes with a few simple modifications such as the addition of a heat and humidity exchange filter to the breathing circuit and the removal of anesthetic gas vaporizers.
Do we need extra resources to make these conversions possible?
An anesthesia professional, such as a certified registered nurse anesthetist, can assist in setting up the machine to be used as a ventilator and should be immediately available at all times to manage the use of the anesthesia machine as a ventilator.
Anesthesia machines must be managed by anesthesia professionals trained in their use and require specific knowledge and skills to optimize their function and to ensure patient safely.
During a crisis when respiratory therapists and other health care providers may be short-staffed or stressed, it is not recommended they be trained to operate new equipment.
How will this take pressure off hospitals that are still scrambling to secure ventilators?
Currently, the FDA has not approved anesthesia machines to be utilized for long-term ventilatory support in an ICU setting, but anesthesia machines can provide life-sustaining mechanical ventilation.
In a crisis such as the COVID-19 pandemic, operating rooms are only being used for emergency surgery, freeing up anesthesia machines to be used as ventilators.
Source: Rutgers University