New research explains why human adults’ heart cells don’t regenerate.
As heart cells mature in mice, the number of communication pathways dramatically decreases, according to a new study.
While this might protect the organ from damaging signals, it could also prevent adult heart cells from regenerating, the researchers found.
The study in Developmental Cell suggests that quieting communication between heart cells and their environment protects the organ from harmful signals related to stresses such as high blood pressure, but at the cost of preventing heart cells from receiving signals that promote regeneration.
“This paper provides an explanation for why adult hearts do not regenerate themselves, but newborn mice and human hearts do,” says senior author Bernhard Kühn, professor of pediatrics and director of the Pediatric Institute for Heart Regeneration and Therapeutics at the University of Pittsburgh School of Medicine and UPMC Children’s Hospital of Pittsburgh.
“These findings are an important advance in fundamental understanding of how the heart develops with age and how it has evolved to cope with stress.”
While skin and many other tissues of the human body retain the ability to repair themselves after injury, the same isn’t true of the heart. During human embryonic and fetal development, heart cells undergo cell division to form the heart muscle. But as heart cells mature in adulthood, they enter a terminal state in which they can no longer divide.
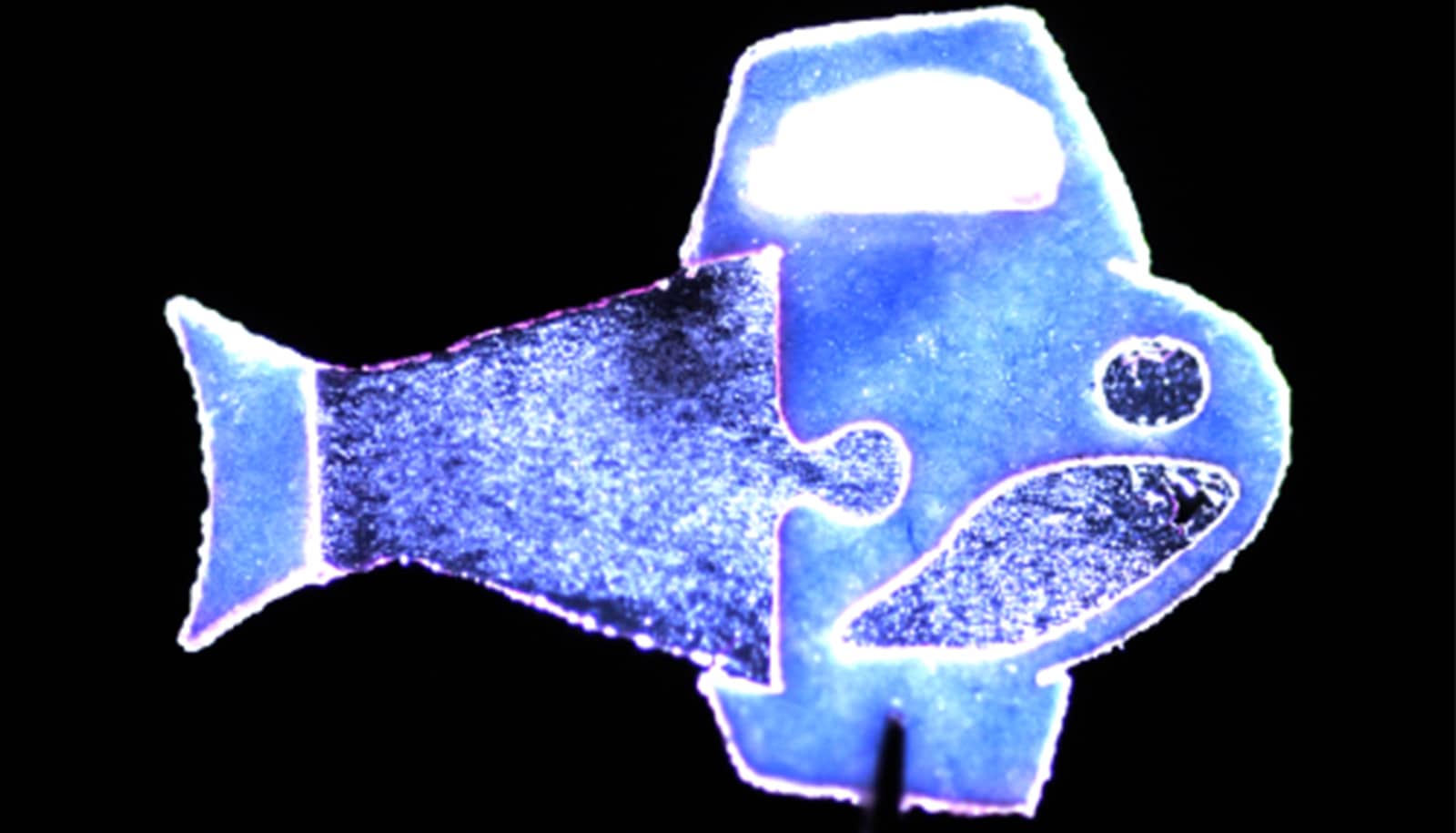
To understand more about how and why heart cells change with age, Kühn teamed up with Yang Liu, associate professor of medicine and bioengineering, and Donna Stolz, associate professor of cell biology and pathology and associate director of the Center for Biologic Imaging, to look at nuclear pores. These perforations in the lipid membrane that surround a cell’s DNA regulate the passage of molecules to and from the nucleus.
“The nuclear envelope is an impermeable layer that protects the nucleus like asphalt on a highway,” says Kühn, who is also a member of the McGowan Institute for Regenerative Medicine. “Like manholes in this asphalt, nuclear pores are pathways that allow information to get through the barrier and into the nucleus.”
Using super-resolution microscopy, Liu visualized and counted the number of nuclear pores in mouse heart cells, or cardiomyocytes. The number of pores decreased by 63% across development, from an average of 1,856 in fetal cells to 1,040 in infant cells to just 678 in adult cells. Stolz validated the findings using electron microscopy to show that nuclear pore density decreased across heart cell development.
In previous research, Kühn and his team showed that a gene called Lamin b2, which is highly expressed in newborn mice but declines with age, is important for cardiomyocyte regeneration.
In the new study, they show that blocking expression of Lamin b2 in mice led to a decrease in nuclear pore numbers. Mice with fewer nuclear pores had diminished transport of signaling proteins to the nucleus and decreased gene expression, suggesting that reduced communication with age may drive a decrease in cardiomyocyte regenerative capacity.
“These findings demonstrate that the number of nuclear pores controls information flux into the nucleus,” explains Kühn. “As heart cells mature and the nuclear pores decrease, less information is getting to the nucleus.”
In response to stress such as high blood pressure, a cardiomyocyte’s nucleus receives signals that modify gene pathways, leading to structural remodeling of the heart. This remodeling is a major cause of heart failure.
The researchers used a mouse model of high blood pressure to understand how nuclear pores contribute to this remodeling process. Mice that were engineered to express fewer nuclear pores showed less modulation of gene pathways involved in harmful cardiac remodeling. These mice also had better heart function and survival than their peers with more nuclear pores.
“We were surprised at the magnitude of the protective effect of having fewer nuclear pores in mice with high blood pressure,” says Kühn. “However, having fewer communication pathways also limits beneficial signals such as those that promote regeneration.”
The Richard King Mellon Foundation Institute for Pediatric Research, HeartFest, the National Institutes of Health, the American Heart Association, the US Department of Defense, the Clinical and Translational Science Institute at Pitt, and the Aging Institute at Pitt and UPMC funded the work.
Source: University of Pittsburgh