Mutations in a gene involved in brain development led researchers to discover two new neurodevelopmental diseases.
The first clues about the rare disorder arose after doctors were unable to diagnose why two siblings from Québec City were experiencing seizures and neurodevelopmental deficits. Desperate, the children’s family turned to Carl Ernst at the Douglas Mental Health University Institute in Montreal for answers.
Ernst, who is also a professor in McGill University’s psychiatry department, and his team used harvested skin cells from the toddlers and “reprogrammed” them to assume a stem cell-like state—induced pluripotent stem cells (iPSC).
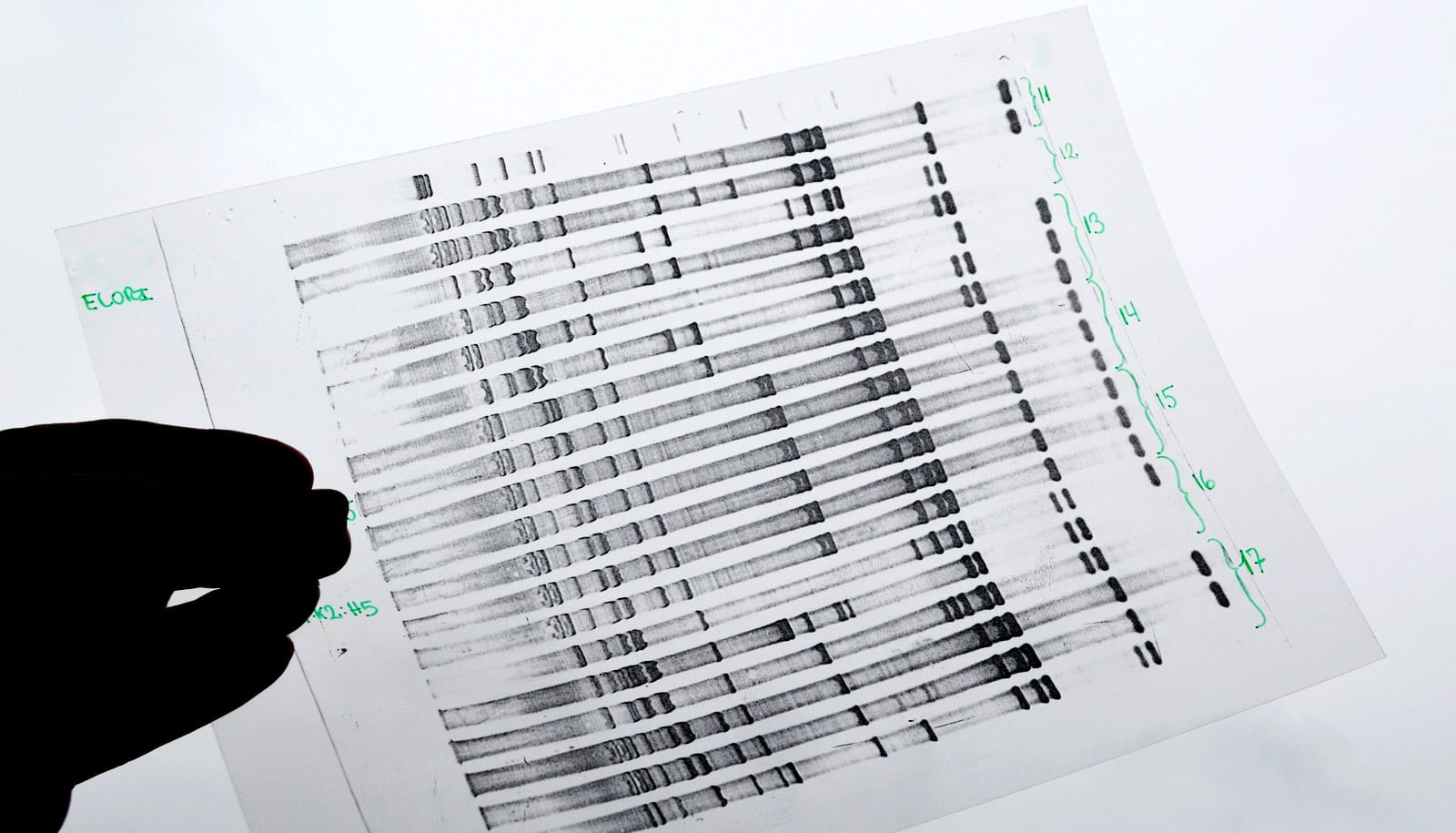
By making neurons from the iPSCs and comparing them to those of healthy individuals, the researchers found that they did not develop properly. Upon further investigation, they discovered a potential culprit: the family carried a mutation in ACTL6B—an epigenetic regulator implicated in neuronal development.
Around the same time, Philippe Campeau, a medical geneticist from CHU Sainte-Justine Research Center, was also studying ACTL6B mutations identified in two families as part of an epilepsy genome study that his colleagues Jacques Michaud and Elsa Rossignol were leading. With the help of Julie Lessard, an ACTL6B expert from the Institute for Research in Immunology and Cancer, Campeau was mapping how ACTL6B mutations affected protein interactions.
After hearing Ernst give a lecture about his work on ACTL6B, Campeau realized they were working on the same mutations so the researchers decided to join forces to study this disease.
By reaching out to peers in over 10 countries, they soon found similar isolated cases throughout the world.
“That’s when we knew that we were looking at a newly identified genetic disease,” says Scott Bell, a PhD student in the Ernst lab and lead author of a new study on the findings in the American Journal of Human Genetics.
As they identified patients with mutations in ACTL6B, the researchers noticed they segregated into two different groups. The first—which had recessive mutations (both copies of the gene are affected) in ACTL6B—suffered from epilepsy and neurodevelopmental problems. The second group—that only had one copy of the gene with mutations—also had problems with neurodevelopment but did not experience seizures. They also showed language delays and hand stereotypies seen in Rett syndrome (caused by mutations in another epigenetic regulator).
“This was very surprising,” says Justine Rousseau, Campeau’s research associate who conducted the protein interaction studies. “It provides very strong evidence that there are in fact two separate neurological genetic diseases caused by mutations in the same gene, ACTL6B.”
Thanks to new research tools such as iPSC and CRISPR gene editing technology, the study shows that ACTL6B mutations caused a dysregulation of other genes important for the development of dendrites, branched projections of neurons that play a critical for communication between brain cells.
Ernst says that their work is concrete proof that new technology is making it easier for scientists to study both rare and neurodevelopmental diseases.
“We’re very happy about this work because concerned families with this disease have, for the first time, a means to understand the problems affecting them,” Ernst says. “The tools we used also provide further evidence of the crucial role ACTL6B plays in brain development and this needs to be further investigated.”
Funding came from the Fonds de recherche en santé du Québec, the government of Indonesia, the Mexican National Council of Science and Technology, MITACS, Genome Canada and Génome Québec, AMED, MEXT, JST, MHLW, the Takeda Science Foundation, and the Canadian Institutes of Health Research.
Source: McGill University