A protein the human body produces naturally could counter the problem of bacterial build-up on medical implants causing infection.
“On any sort of device that you try to put in a human, a biofilm will form.”
Artificial hip implants, knee implants, and catheters are all susceptible to infections. Bacteria that flow through the blood system can collect on these foreign surfaces and hunker down to proliferate.
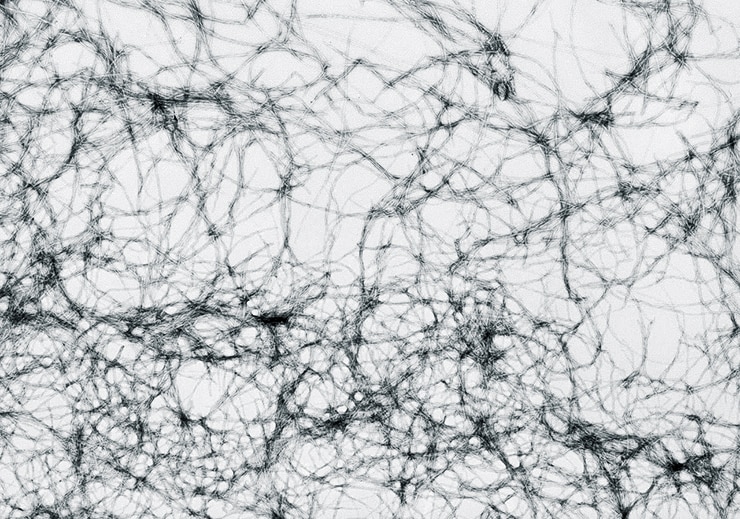
When bacteria collect on a surface, they form a protective layer called a biofilm. A scaffolding composed of a protein called amyloid that the bacteria itself produces holds these biofilms together. The bacterial amyloid is similar to the structure that snarls neurons in the brains of people with Alzheimer’s disease, disrupting the person’s ability to form and recall memories.
In the case of bacteria on a prosthetic, biofilms protect the colony of bacteria from its environment, including from antibiotics a doctor might prescribe to attack the infection.
In a new study, the researchers found that a protein produced by humans called transthyretin, or TTR, can suppress the formation of amyloid and biofilm in E. coli, a common bacterial strain found in humans.
Breaking sticks, not the bundle
“One of the most important health implications for biofilms is on catheters. On any sort of device that you try to put in a human, a biofilm will form,” says Matthew Chapman, professor of molecular, cellular, and developmental biology at the University of Michigan. “This is a huge, huge problem because being catheterized for just a few days, bacteria can form biofilms on the device, which can lead to serious infections.”
“It’s easier to break individual sticks rather than a bundle…”
The team studied how TTR interacted with a strain of E. coli found in urinary tract infections. In UTIs, the bacterial strain settles into the bladder, forming biofilm communities. Bacteria in a biofilm encase themselves in a coat of amyloid fibers that help to protect them from stressors in the environment. E. coli amyloids are composed of a protein called CsgA.
When the researchers mixed purified TTR and CsgA, CsgA could not make protective amyloids. Taking down a bacteria’s key defense against its environment could allow the body to fight the infection more effectively.
“It’s easier to break individual sticks rather than a bundle. Similarly, bacterial infections can be dealt more effectively if bacteria are not held together in biofilms,” says lead author Neha Jain, a postdoctoral fellow in the Chapman lab. “We found that TTR can prevent biofilm formation in a uropathogenic E. coli strain as well as other bacterial strains.”
Use biofilm’s own enzymes to defeat its ‘armor’
Joel Buxbaum, a professor of molecular medicine with TSRI who has long studied TTR, pointed out that under some conditions TTR can form amyloid fibers itself, and it could be this ability that gives TTR the structural characteristics to interrupt amyloid formation by other proteins, such as CsgA.
Potential impact
About one in 100 people who receive hip or knee replacements experience an infection, according to the American Academy of Orthopaedic Surgeons. A 2001 study found that 95 percent of urinary tract infections in critically ill patients were traced back to their catheters, while 87 percent of bloodstream infections came from an indwelling vascular catheter and 86 percent of pneumonia cases were associated with a mechanical ventilator.
“It’s possible that products derived or based on these protein interactions could reduce this problem in medicine, that biofilms form on a lot of artificial surfaces implanted within the body,” Buxbaum says.
“The notion is we could impregnate these surfaces with this protein so that they may not form these biofilms and make it easier to treat these infections with antibiotics,” he explains.
Chapman and Buxbaum say implementing this will require more research, but the move could help prevent infections on implants as well as antibiotic resistance.
“If you could target that resistance, the host may be able to clear the infection,” Chapman says. “You could also potentially prescribe lower doses of antibiotics or shorten the duration of antibiotic usage, which would all be good things.”
Trick bacteria’s little ‘limbs’ to stop a biofilm
The researchers reported their findings in the Proceedings of the National Academy of Science.
Source: University of Michigan



