Researchers have optimized a new method to create synthetic neurons, neuron-like cells created from a readily available cell line.
They also used these cells to investigate a core enzyme involved in the synthesis of purines—a component of DNA that is involved in many other cellular and metabolic processes—and how the enzyme might change during infection by herpes simplex virus.
An early version of the paper describing the enzyme appears in the Journal of Neurochemistry, and a paper describing the neuron-like cells appears in the Journal of Virology.
Opening new doors
“These newly developed neuron-like cells allowed us to investigate purine formation in a specialized cell type for the first time,” says Moriah Szpara, assistant professor of biochemistry and molecular biology at Penn State and senior author of both papers.
“[These cells] provide a new avenue to study how neurons respond to neurotropic viruses, like HSV, HIV, rabies, West Nile, Zika, and Chikungunya.”
“We were interested in neurons because they require a lot of energy and therefore need to produce purines efficiently. We were also curious how the synthesis process might be affected by infection with herpes simplex virus, an energetically demanding virus that takes up residence in neurons,” Szpara says.
When demand for purines is high in a cell, a complex composed of many enzymes called the purinosome forms to enable faster production of these important chemicals.
The researchers investigated an enzyme called FGAMS, a core component of the purinosome. To better understand the role of FGAMS in purine production, they looked at where and how much of the enzyme is expressed in rodent brain slices, rodent neurons, human non-neuronal cells, and the human neuron-like cells cultivated with the new technique.
“Studying human neurons has been challenging because we haven’t had a good laboratory model to study them,” says Colleen Mangold, a postdoctoral researcher at Penn State and an author of both studies.
“We can use neurons from rodents or chick embryos, but they don’t give us the same information as human cells. Most studies require large numbers of cells, so we developed a method to take a commonly available cell line and shape it into cells that look and act like neurons. This new method will allow us to start asking the backlog of questions we have about neurons, like how purines are synthesized in the brain,” Mangold says.
In the neuron-like cells and in rodent neurons and brain slices, FGAMS was expressed in a number of locations throughout the neuron, including near mitochondria and microtubules. Because FGAMS is also found near these structures in non-neuronal cells, the researchers suspect that purinosome formation may be conserved across different cell types.
Investigating viral infections
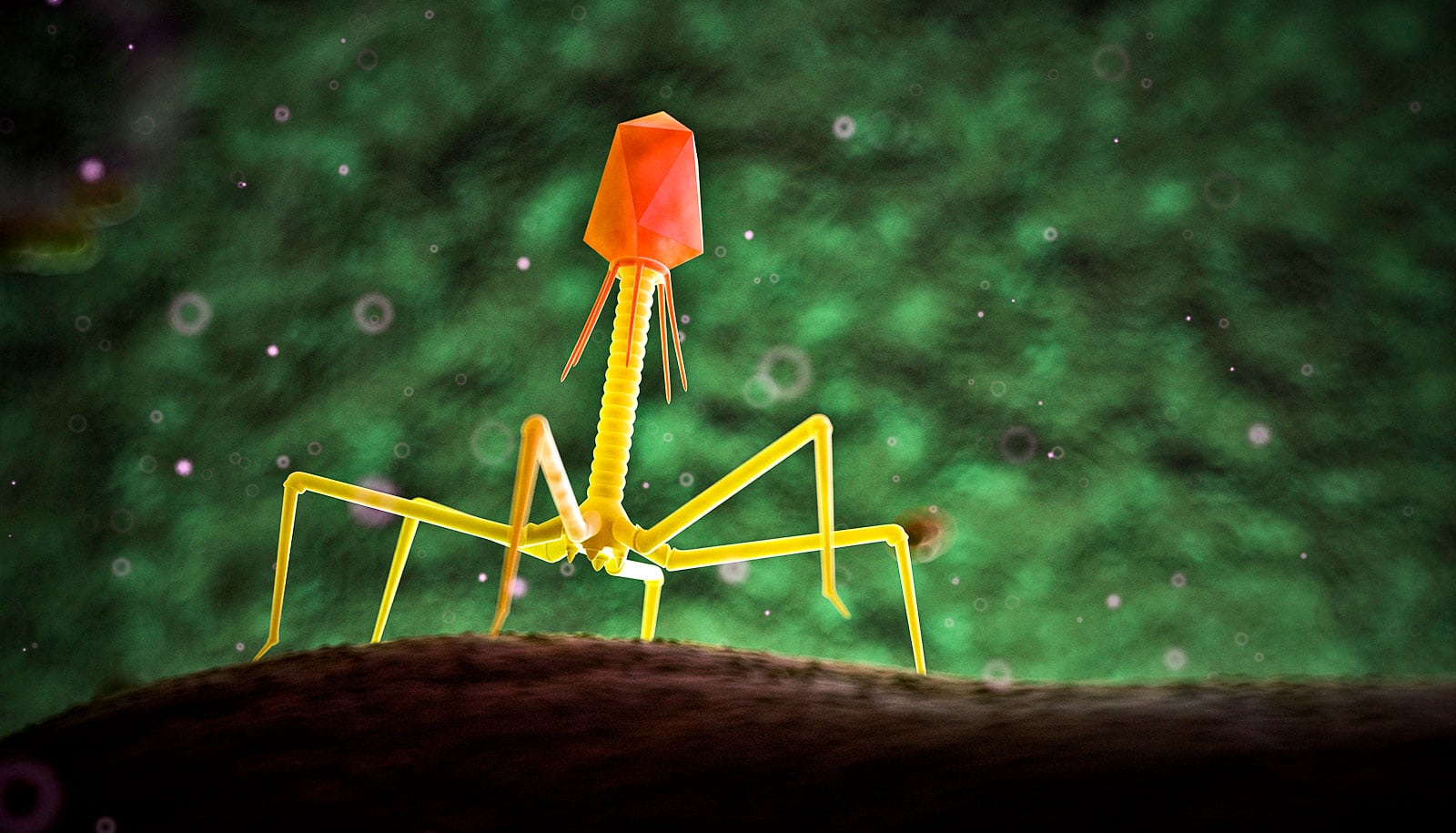
The researchers also investigated the effect of infection with herpes simplex virus 1 (HSV1) on the purine biosynthesis protein FGAMS both in neurons and in non-neuronal cells. HSV1 initially infects an individual at the skin surface and proceeds to set up a lifelong infection in neurons that cannot be cleared by the immune system. Because purines may play a role in the replication of HSV1, the high metabolic load of the virus might deplete purine resources and affect purine synthesis.
Scientists create new motor neurons out of skin cells
“Infection with HSV1 induced clustering of FGAMS in the non-neuronal cells, which model the skin phase of infection, while FGAMS appeared to be constantly clustered and activated in neuronal cells,” says Stephen Benkovic, professor of chemistry and an author of the purine formation paper.
“We suspect that the purinosome is assembled only on an as-needed basis in non-neuronal cells, but that high energetic demands in neurons may necessitate the purinosome being present all of the time,” Benkovic says.
“Viruses like HSV1 survive by establishing a lifelong infection in neurons,” says Szpara, “and there is growing evidence suggesting links between chronic viral infections and late-life neurocognitive diseases. We are continuing to investigate the potential connections between the burdens of viral infection and the high metabolic demands of neurons to see if there are avenues to prevent damage and improve long-term neuronal health.”
Because the results from the neuron-like cells mirror those in the rodent brain slices and neurons, the study highlights the utility of these cells as a new model system for studying neurons and how viruses affect them.
“These neuron-like cells are easy to grow in great numbers and will allow us to capture some of the nuance we missed when studying viruses in non-neuronal cells,” says graduate student Mackenzie Shipley, first author of the synthetic neuron paper. “While these cells can be used to ask a variety of questions about neurons, they also provide a new avenue to study how neurons respond to neurotropic viruses, like HSV, HIV, rabies, West Nile, Zika, and Chikungunya.”
DART sends drugs to some neurons, not others
In addition to Szpara, Mangold, and Benkovic, the research team on the project exploring the formation of purines includes Pamela Yao of the National Institutes of Health (NIH) National Institute of Aging, and Mei Du and Willard Freeman of the University of Oklahoma Health Sciences Center. The funding from this work came, in part, from NIH, the American Heart Association, the NIH National Institute of Aging, the Huck Institutes of the Life Sciences at Penn State, and the Pennsylvania Department of Health Commonwealth Universal Research Enhancement (CURE) program.
In addition to Szpara, Mangold, and Shipley, the research team on the project describing the neuron-like cells includes Chad Kuny, postdoctoral researcher at Penn State. Funding for this work came from the NIH National Institute of Allergy and Infectious Diseases (NAID) Virus Pathogens Resource (ViPR) Bioinformatics Resource Center, and is supported by the Huck Institutes of the Life Sciences.
Source: Penn State