Adherence to the guidelines is low among US gastroenterologists treating patients with H. pylori, survey results show.
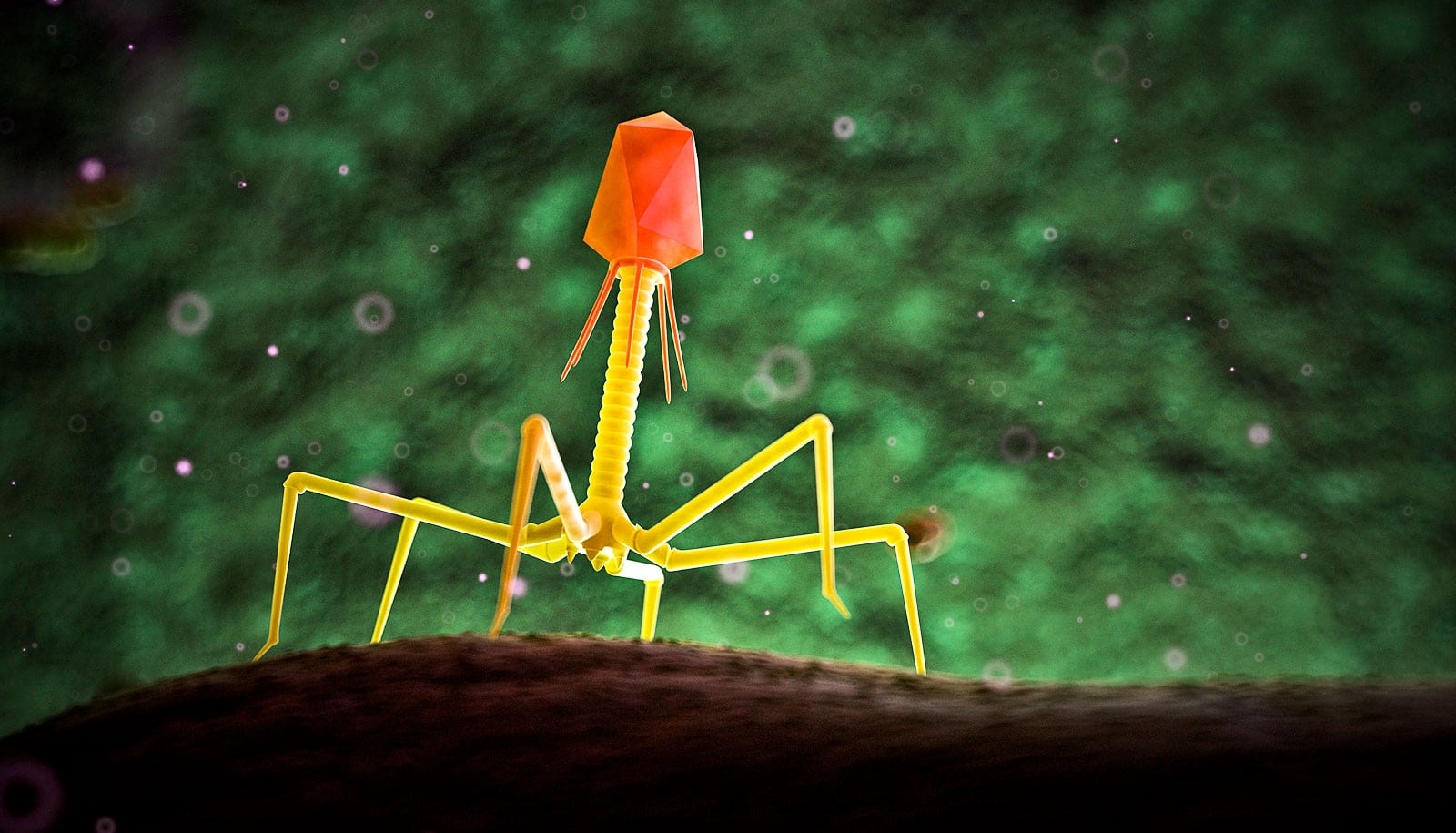
Stress was once the assumed cause of gastric ulcers and other digestive maladies. But in 2005, Barry J. Marshall and J. Robin Warren received the Nobel Prize in Physiology or Medicine for recognizing the role of Helicobacter pylori in gastritis and peptic ulcer disease. Now physicians can blame it when it comes to a host of gastric maladies in their patients.
With this in mind, researchers conducted a study into whether US physicians consistently adhere to American College of Gastroenterology guidelines for caring for and managing patients with H. pylori infections. Guidelines include when and how to test for H. pylori, as well as when and how to treat the pathogen once someone has been infected.
Caring for and managing these patients is important not only because of the serious potential morbidity associated with H. pylori infections, but also because these infections are linked to gastric cancer. The results are published in the journal Preventive Medicine.
Most physicians follow the guidelines for testing patients they suspect of having H. pylori infection when the patients came to them with likely risk factors, such as a previously diagnosed peptic ulcer or dyspepsia.
“You shouldn’t be testing everybody, but if there are reasons to believe that a test for H. pylori may come back positive, and it does come back positive, you should go on to treat,” says lead author Traci Murakami, previously a gastroenterology fellow at the University of Arizona and now an assistant clinical professor of medicine at the University of Hawaii, Manoa.
Video of H. pylori swimming in ‘broth’ offers clues about ulcers
In fact, the researchers found that a higher proportion of physicians than in years past treat patients after a positive H. pylori test, with 84 percent of the respondents indicating they would do so, says Eyal Oren, assistant professor of epidemiology at the University of Arizona’s Mel and Enid Zuckerman College of Public Health.
However, only 58 percent of physicians checked to make sure the bacterium has been eradicated after treatment. This finding is of particular concern, Murakami says, because if the bacterium is not eradicated after the recommended therapy, it could indicate potential resistance to drugs of choice.
“Only half of gastroenterology physicians check for eradication,” Murakami says. “I think that’s key because knowing if a patient eradicated the H. pylori versus whether they still have the infection may indicate that they may have a more resistant type of H. pylori that didn’t respond to the initial antibiotic and would require different antibiotics to eradicate it.”
Also of concern, 6 percent of physicians weren’t asking patients about antibiotics that they previously had taken. That information could be an alert about the potential for drug resistance. Further, many physicians aren’t testing for resistance, perhaps because doing so isn’t cheap or easy.
While some people are colonized with H. pylori from birth and experience no ill effects from it until much later in life, if at all, some researchers have called for its global eradication, saying “adaptation of a ‘test, treat, and retest strategy’ to confirm eradication after treatment is an area that could be improved.”
Further, the World Health Organization has designated it a carcinogen.
“If we could identify it early and identify it in more people, we might be able to reduce the risk of people developing stomach cancer in the future,” Murakami says.
The Art Chapa Foundation for Gastric Cancer Prevention funded the work.
Source: University of Arizona