SARS-CoV-2, the virus that causes COVID-19, can relieve pain, according to a new study.
The finding may explain why nearly half of all people who get COVID-19 experience few or no symptoms, even though they can spread the disease, says Rajesh Khanna, a professor in the University of Arizona College of Medicine-Tucson.
“It made a lot of sense to me that perhaps the reason for the unrelenting spread of COVID-19 is that in the early stages, you’re walking around all fine as if nothing is wrong because your pain has been suppressed,” Khanna says.
“You have the virus, but you don’t feel bad because your pain is gone. If we can prove that this pain relief is what is causing COVID-19 to spread further, that’s of enormous value.”
The US Centers for Disease Control and Prevention released updated data September 10, estimating that 50% of COVID-19 transmission occurs prior to the onset of symptoms and 40% of COVID-19 infections are asymptomatic.
“This research raises the possibility that pain, as an early symptom of COVID-19, may be reduced by the SARS-CoV-2 spike protein as it silences the body’s pain signaling pathways,” says Michael D. Dake, senior vice president at University of Arizona Health Sciences.
“University of Arizona Health Sciences researchers at the Comprehensive Pain and Addiction Center are leveraging this unique finding to explore a novel class of therapeutics for pain as we continue to seek new ways to address the opioid epidemic.”
SARS-CoV-2 and pain relief
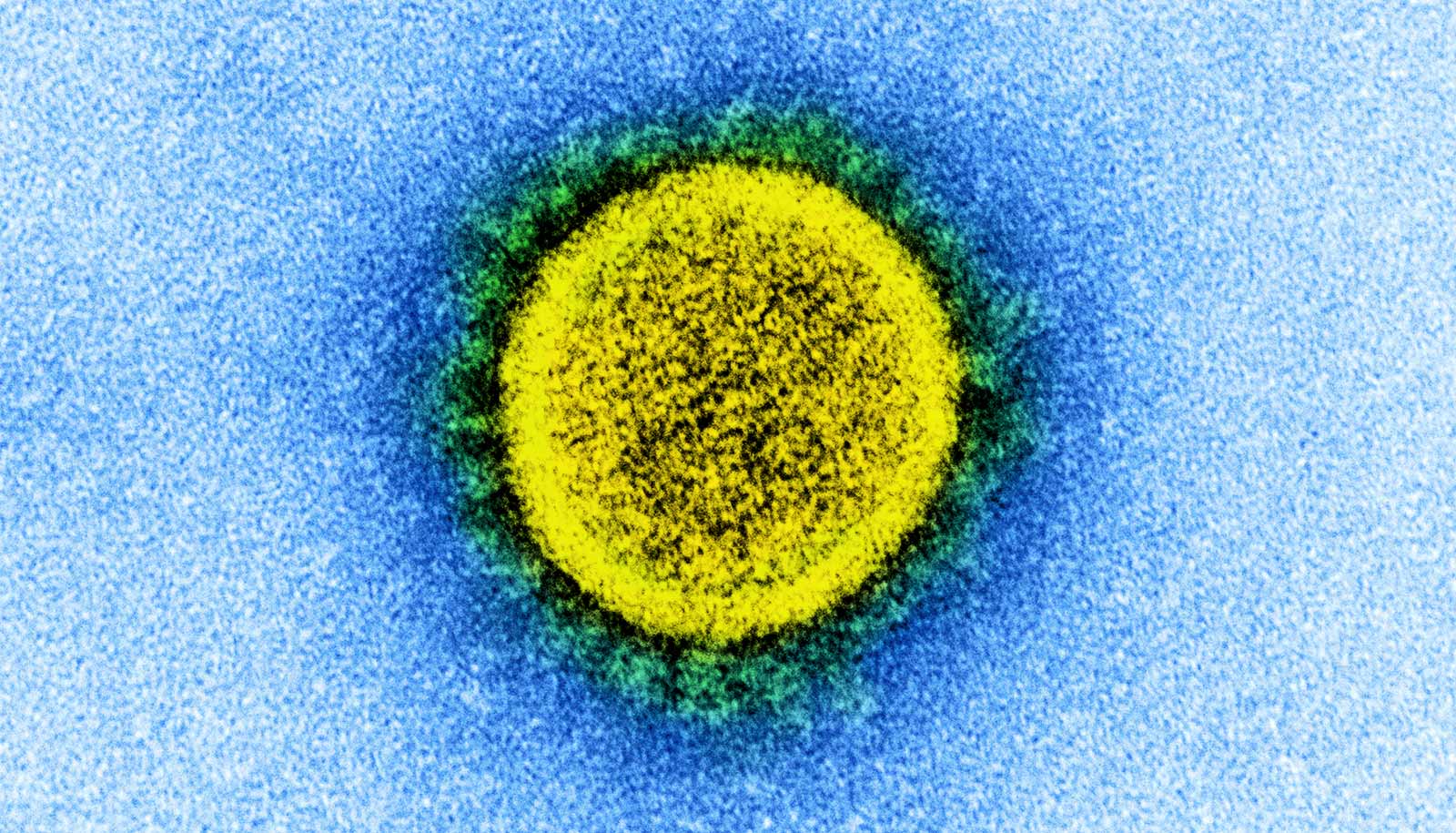
Viruses infect host cells through protein receptors on cell membranes. Early in the pandemic, scientists established that the SARS-CoV-2 spike protein uses the angiotensin-converting enzyme 2 (ACE2) receptor to enter the body. But in June, two papers posted on the preprint server bioRxiv pointed to neuropilin-1 as a second receptor for SARS-CoV-2.
“That caught our eye because for the last 15 years, my lab has been studying a complex of proteins and pathways that relate to pain processing that are downstream of neuropilin,” says Khanna. “So we stepped back and realized this could mean that maybe the spike protein is involved in some sort of pain processing.”
“We have a pandemic, and we have an opioid epidemic. They’re colliding. Our findings have massive implications for both.”
Many biological pathways signal the body to feel pain. One works through a protein named vascular endothelial growth factor-A (VEGF-A), which plays an essential role in blood vessel growth but also has been linked to diseases such as cancer, rheumatoid arthritis, and, most recently, COVID-19.
Like a key in a lock, when VEGF-A binds to the receptor neuropilin, it initiates a cascade of events resulting in the hyperexcitability of neurons, which leads to pain. Khanna and his research team found that the SARS-CoV-2 spike protein binds to neuropilin in exactly the same location as VEGF-A.
With that knowledge, they performed a series of experiments in the laboratory and in rodent models to test their hypothesis that the SARS-CoV-2 spike protein acts on the VEGF-A/neuropilin pain pathway. They used VEGF-A as a trigger to induce neuron excitability, which creates pain, then added the SARS-CoV-2 spike protein.
“The spike protein completely reversed the VEGF-induced pain signaling,” Khanna says. “It didn’t matter if we used very high doses of spike or extremely low doses—it reversed the pain completely.”
Pandemic-opioid epidemic collision
Khanna is teaming up with immunologists and virologists to continue research into the role of neuropilin in the spread of COVID-19.
In his lab, he will examine neuropilin as a new target for non-opioid pain relief. During the study, Khanna tested existing small molecule neuropilin inhibitors developed to suppress tumor growth in certain cancers and found they provided the same pain relief as the SARS-CoV-2 spike protein when binding to neuropilin.
“We are moving forward with designing small molecules against neuropilin, particularly natural compounds, that could be important for pain relief,” Khanna says.
“We have a pandemic, and we have an opioid epidemic. They’re colliding. Our findings have massive implications for both. SARS-CoV-2 is teaching us about viral spread, but COVID-19 has us also looking at neuropilin as a new non-opioid method to fight the opioid epidemic.”
The study appears in the journal PAIN.
Source: University of Arizona