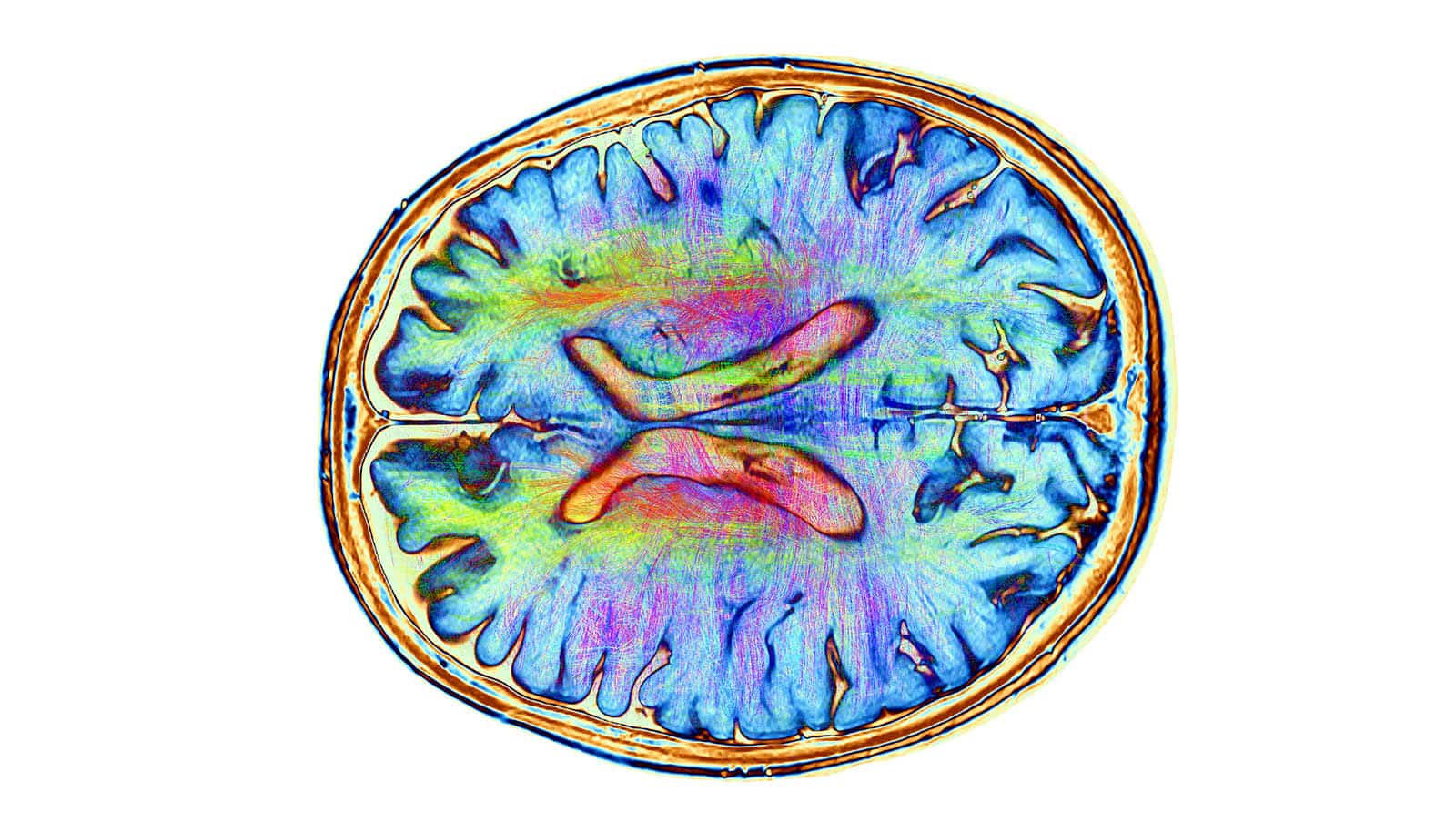
A new tool for noninvasive imaging can help illuminate hard-to-access structures and processes in the brain.
The small-molecule dye, or fluorophore, is the first of its kind that can cross the blood-brain barrier. What’s more, it allowed the researchers to differentiate between healthy brain tissue and a glioblastoma tumor in mice.
“This could be very useful for imaging-guided surgery, for example,” says Han Xiao, assistant professor of chemistry, biosciences, and bioengineering at Rice University. “Using this dye, a doctor could determine where the boundary is between normal brain tissue versus tumor tissue.”
If you’ve been to an aquarium or a nightclub, you’ve probably noticed the colorful glow that some objects or surfaces emit under a black light. Known as fluorescence, this glowing effect can be useful for rendering visible things that otherwise go unnoticed.
“Fluorescence imaging has been applied for imaging cancer in different parts of our body,” Xiao says. “The advantages of a fluorescence probe include high resolution and the ability to adapt the probe to read for different substances or activities.”
The deeper a tissue or organ is, the longer the wavelengths needed to discern the presence of fluorescent small molecules. For this reason, the second near-infrared (NIR-II) channel with wavelengths of 1,000 to 1,700 nanometers is especially important for deep-tissue imaging. For reference, visible light wavelengths range from 380 to 700 nanometers.
“Our tool is really valuable for deep imaging because it functions in the NIR-II region,” Xiao says. “In contrast to NIR-II wavelengths, fluorescent effects within the visible spectrum or with near-infrared wavelengths between 600 and 900 nanometers (NIR-I) will only get you skin-deep.”
Brain imaging poses a particular challenge not only because of tissue depth and accessibility, but also because of the blood-brain barrier, a layer of cells that acts as a very selective filter to restrict the passage of substances from the circulatory system to the central nervous system.
“People always want to know what exactly is happening in the brain, but it’s very hard to design a molecule that can penetrate the blood-brain barrier. Up to 98% of small-molecule drugs approved by the Food and Drug Administration (FDA) cannot,” Xiao says.
“Generally speaking, the reason a NIR-II dye molecule tends to be big is because it is a conjugated structure with many double bonds,” he continues. “This is a true problem and the reason why we have been unable to use fluorescence in brain imaging until now. We tried to address this issue by developing this new dye scaffold that is very small but has a long emission wavelength.”
Unlike the other two known NIR-II dye scaffolds, which are not capable of crossing the blood-brain barrier, the one Xiao and Zhen Cheng of Stanford University developed is more compact, which makes it a great candidate for probes or drugs targeting the brain. “In the future, we could modify this scaffold and use it to look for a lot of different metabolites in the brain,” Xiao says.
Beyond the brain, the dye has much greater lasting power than indocyanine green, the only NIR small-molecule dye approved by the FDA for use as a contrast agent. A longer lifespan means researchers have more time to record the fluorescent trace before it disappears.
“When exposed to light, the indocyanine green dye trace deteriorates in seconds, whereas our dye leaves a stable trace for more than 10 minutes,” Xiao says.
The study appears in the Journal of the American Chemical Society.
Support was provided by the Cancer Prevention Research Institute of Texas, the National Institutes for Health, the Department of Defense, the Robert A. Welch Foundation, the National Science Foundation, a Hamill Innovation Award, the John S. Dunn Foundation Collaborative Award, and the Stanford University Department of Radiology.
Source: Rice University