Measuring the quantity of influenza-specific antibodies in a person’s blood may show if they had the flu, but also possibly when they experienced the virus. This information could improve the way doctors monitor influenza, particularly in places where flu season does not end.
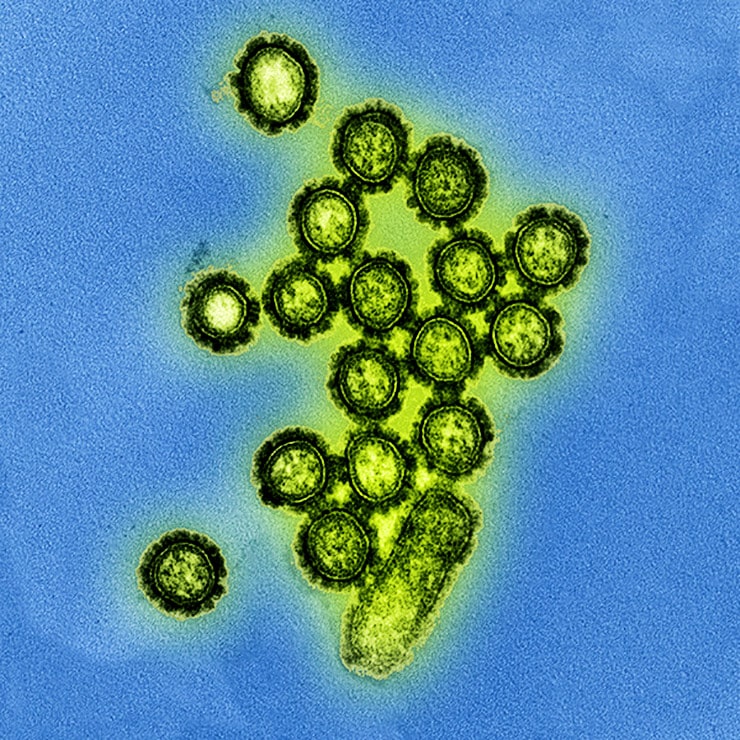
In a new study, researchers found that they could identify concentrations of antibodies that corresponded to recent and past exposure to the flu strain H1N1—the strain involved in the 2009 flu pandemic.
“Disease outbreaks and epidemics are often monitored by counting individuals who show symptoms of infection, but this only captures people who are sick enough to be identified,” says Maciej Boni, associate professor of biology at Penn State and a lead author of the paper.
“With blood samples, you can capture everyone that ever was infected because individuals are not able to hide their antibody signals,” he says.
Antibodies defend against viral attack, and their numbers spike in the presence of an infection like influenza. Approximately one month after infection, the number of flu-specific antibodies in the blood begins to decrease, but some antibodies continue to circulate long after the virus has cleared.
In the past, scientists have measured the concentration of antibodies remaining to identify whether an individual has been exposed to the virus, but the results of these tests have typically been limited to describing the presence or absence of past infection.
“This work will help us assess who is most at risk during a new influenza outbreak…”
“In this study we showed that there is a lot more information in measurements of antibody concentration than just presence or absence,” says Boni. “Our results show that antibody concentration should be able to provide information about the timing of past influenza infection.”
This information is especially valuable in tropical climates. “In temperate regions like the United States, we might collect blood samples when the flu season is over to see what percentage of people were infected during that flu season,” Boni explains. “But in the tropics there is no flu season—it may be constantly circulating or it could come in waves. If all you measure is the presence or absence of antibodies, you can’t determine when those individuals were infected.”
The research team analyzed over 20,000 blood samples from four hospitals in southern Vietnam, taken every two months between 2009 to 2013.
“This is the largest study of its kind, and custom statistical methods needed to be developed for this analysis,” says Nguyen Thi Duy Nhat, a graduate student at the Oxford University Clinical Research Unit at the time of the study and first author of the paper. This immense undertaking will allow the team to map out the H1N1 flu strain’s dynamics in the tropics in the next phase of their research.
“The 2009 influenza pandemic taught us the importance of understanding the history of exposure in the community as a factor of a pandemic’s impact,” says Marion Koopmans, head of the viroscience department at the Erasmus Medical Centre and a lead author of the study.
“Here, we introduce a novel approach that measures a population’s exposure history to currently circulating viruses. This work will help us assess who is most at risk during a new influenza outbreak,” she says.
Stronger flu vaccine may keep seniors out of hospital
The research team defined four categories of H1N1-specific antibody concentrations. The highest concentrations indicate exposure to H1N1 within the last six months, the second highest concentrations indicate exposure greater than six months prior, and the lowest two categories of concentrations indicate no previous exposure to the virus.
Use of these categories could allow public health officials in other tropical locations to determine infection rates of H1N1 with systematic sampling, for example, by screening a subset of the population every January to determine the previous year’s infection rate.
The researchers used a protein microarray—a high-throughput large-scale test that measures interactions of large numbers of proteins in parallel—to measure antibody concentrations. Developed in the Netherlands, this relatively new technique allows precise antibody measurements with very small volumes of blood.
“This protein microarray has high reproducibility and can provide specificity to 16 different influenza strains,” says Erwin de Bruin, senior laboratory technician at Erasmus Medical Centre and an author of the study. “The small volume of blood required provides a simpler way to perform large epidemiological studies.”
“This microarray, and the additional information about time of infection from antibody concentrations, could change how we monitor disease in the tropics,” adds Boni.
“Currently, public health systems monitor antibodies after an outbreak or for the purpose of research, but most of the monitoring effort focuses on symptoms through hospital-based surveillance,” Boni says. “By next decade, we may be able to perform regular surveillance of blood, which would give us a better picture of the diseases circulating through a population. This kind of surveillance is especially important in tropical countries where a lot of novel viruses emerge.”
The 5 biggest myths about the flu
A paper describing the research appears in the journal Scientific Reports.
Additional researchers contributing to this work are from the Oxford University Clinical Research Unit in Ho Chi Minh City, Vietnam; the Erasmus Medical Centre in Rotterdam, Netherlands; and Penn State.
The Wellcome Trust and the British Medical Association funded the research, supported by the National Health and Medical Research Council of Australia and the Dutch Ministry of Economic Affairs, Agriculture, and Innovation Castellum Project.
Source: Penn State



