Cancer cells may develop resistance to drugs known as checkpoint inhibitors by simply getting rid of mutations that would otherwise trigger the body’s disease-fighting immune system, research suggests.
Researchers conducted the study, aimed at determining why so-called immunotherapy can become ineffective over time, on cells from five lung cancer and head and neck cancer patients. A summary appears online in the journal Cancer Discovery.
“When the cancer cells shed these mutations, they discard the evidence that would normally lead them to be recognized by the body’s protective immune cells.”
“Our findings offer evidence about how cancer cells evolve during immunotherapy,” says Victor E. Velculescu, professor of oncology at Johns Hopkins University and a leader of the research. “When the cancer cells shed these mutations, they discard the evidence that would normally lead them to be recognized by the body’s protective immune cells.”
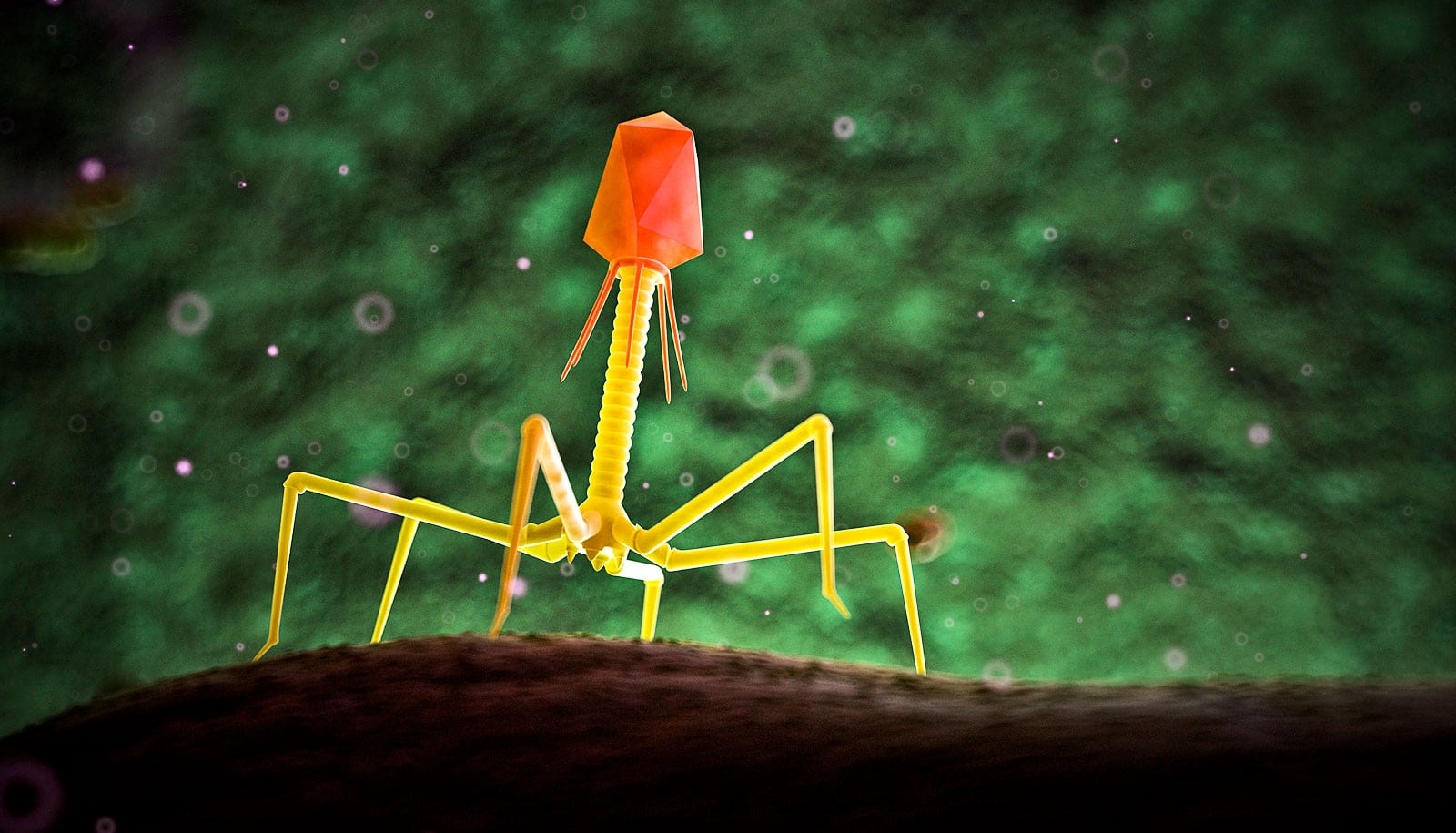
Checkpoint inhibitors are approved by the FDA for use against lung cancer, metastatic melanoma, head and neck cancer, and Hodgkin lymphoma. The drugs reveal evidence of mutated proteins on the surface of cancer cells, helping the patient’s own immune system recognize and attack cancer.
“Checkpoint inhibitors are one of the most exciting recent advances for cancers, but the mechanism by which most patients become resistant to these therapies has been a mystery,” Velculescu says.
Toxin and anti-toxin let some bacteria evade antibiotics
To investigate, Velculescu, oncology instructor Valsamo Anagnostou, research associate Kellie N. Smith, and their colleagues studied tumors from patients who developed resistance to two checkpoint inhibitors: a drug called nivolumab that uses an antibody called anti-PD-1, and nivolumab in combination with ipilimumab, which uses an antibody called anti-CTLA4.
Using biopsies of tumors collected before the start of treatment and when patients developed resistance, the researchers performed large-scale genomic analyses to search for mutations specific to the cancer cells in all of each patient’s 20,000 genes.
The search narrowed down to mutations in genes that code for antigens, producing misshapen or otherwise altered antigens called neoantigens. Such neoantigens are seen by the immune system as foreign threats, and thus, the cancer cell is flagged for destruction, usually with the help of immunotherapy drugs.
The scientists found that by the time the patients developed resistance to immunotherapy, their tumors had shed between seven and 18 mutations in neoantigen-coding genes. Without those mutations, the tumor cells’ neoantigens look less foreign to the immune system and might go unrecognized, the scientists say.
Nontoxic strain of Salmonella tested as cancer treatment
The researchers found that the tumors had lost these mutations by various means, including deleting large regions of chromosomes in all cancer cells.
“In some instances,” says Anagnostou, “we found that chromosomes in the cancer cells’ nuclei were missing an entire arm containing these mutated genes.”
The team plans to determine how broadly this phenomenon occurs in other cancer types and develop ways to improve current cancer immunotherapies. For example, they say, mutated neoantigens present in tumor cells before therapy could give clues as to which patients might develop resistance. The findings could also advance development of new checkpoint inhibitors less likely to trigger resistance.
Four checkpoint inhibitors are currently approved by the FDA—nivolumab, pembrolizumab, atezolizumab, and ipilimumab—to treat melanoma, lymphoma, bladder, lung and head and neck cancers. The drugs cost more than $10,000 per month, an expense that has fueled efforts to improve their efficiency.
The National Cancer Institute, the Commonwealth Foundation, the Dr. Miriam and Sheldon G. Adelson Medical Research Foundation, the Eastern Cooperative Oncology Group-American College of Radiology Imaging Network, the LUNGevity Foundation, and Stand Up to Cancer funded the work.
Source: Johns Hopkins University